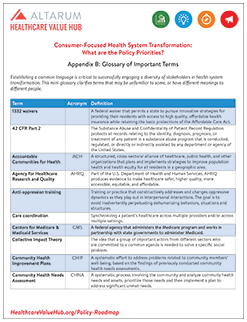
Consumer-Focused Health System Transformation:
What are the Policy Priorities?
Appendix B - Glossary of Terms
Establishing a common language is critical to successfully engaging a diversity of stakeholders in health system transformation. This mini-glossary clarifies terms that may be unfamiliar to some, or have different meanings to different people.
|
Term |
Acronym |
Definition |
|
1332 waivers |
A federal waiver that permits a state to pursue innovative strategies for providing their residents with access to high quality, affordable health insurance while retaining the basic protections of the Affordable Care Act. |
|
|
42 CFR Part 2 |
The Substance Abuse and Confidentiality of Patient Record Regulation protects all records relating to the identity, diagnosis, prognosis, or treatment of any patient in a substance abuse program that is conducted, regulated, or directly or indirectly assisted by any department or agency of the United States. |
|
|
Accountable Communities for Health |
ACH |
A structured, cross-sectoral alliance of healthcare, public health, and other organizations that plans and implements strategies to improve population health and health equity for all residents in a geographic area. |
|
Agency for Healthcare Research and Quality |
AHRQ |
Part of the U.S. Department of Health and Human Services, AHRQ produces evidence to make healthcare safer, higher quality, more accessible, equitable, and affordable. |
|
Anti-oppression training |
Training or practice that constructively addresses and changes oppressive dynamics as they play out in interpersonal interactions. The goal is to avoid inadvertently perpetuating dehumanizing behaviors, situations and structures. |
|
|
Care coordination |
Synchronizing a patient’s healthcare across multiple providers and/or across multiple settings. |
|
|
Centers for Medicare & Medicaid Services |
CMS |
A federal agency that administers the Medicare program and works in partnership with state governments to administer Medicaid. |
|
Collective Impact Theory |
The idea that a group of important actors from different sectors who are committed to a common agenda is needed to solve a specific social problem. |
|
|
Community Health Improvement Plans |
CHIP |
A systematic effort to address problems related to community members’ well-being, based on the findings of previously conducted community health needs assessments. |
|
Community Health Needs Assessment |
CHNA |
A systematic process involving the community and analyze commuity health needs and assets, prioritize those needs and then implement a plan to address significant unmet needs. |
|
Coordinated Care Organization |
CCO |
A network of healthcare providers (physical healthcare, addictions and mental healthcare and dental care providers) who work together in their local communities to serve people who receive healthcare coverage under the Oregon Health Plan. |
|
Critical Access Hospitals |
CAH |
A federal designation given to eligible rural hospitals designed to reduce the financial vulnerability of rural hospitals and improve access to healthcare by keeping essential services in rural communities. CAHs receive certain benefits, such as cost-based reimbursement for Medicare services. |
|
Federally Qualified Health Centers |
FQHC |
Community-based healthcare providers that receive funds from the HRSA Health Center Program to provide primary care services in underserved areas. |
|
Employee Retirement Income Security Act |
ERISA |
A federal law that sets minimum standards for most retirement and health plans in private industry to provide protection for individuals in these plans. |
|
Fee-for-service |
FFS |
A payment model in which providers are paid for every unit of service delivered without consideration of quality, outcomes or efficiency. |
|
Graduate Medical Education |
GME |
Refers to any type of formal medical education, usually hospital-sponsored or hospital-based training, pursued after receipt of a M.D. or D.O. degree. The Medicare program provides direct and indirect funding to help teaching hospitals cover costs directly related to educating physician residents. Indirect GME funding accounts for the higher costs of complex patients treated by these hospitals. |
|
Health equity |
Attainment of the highest level of health for all people; requires valuing everyone equally, with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and healthcare disparities. |
|
|
Health-related social needs |
Refers to the social determinants that have a near-term impact on health. |
|
|
Health Insurance Portability and Accountability Act |
HIPAA |
A federal law that promises continued health insurance coverage and ensures health information privacy for those covered by health insurance plans. |
|
Health Resources & Services Administration |
HRSA |
The primary federal agency for improving healthcare to people who are geographically isolated, economically or medically vulnerable. |
|
Internal Revenue Service |
IRS |
The nation’s tax collection agency. |
|
National Health Service Corps |
NHSC |
Operated by HRSA; builds healthy communities by supporting qualified healthcare providers dedicated to working in areas of the United States with limited access to care. |
|
National Institutes of Health |
NIH |
Part of the U.S. Department of Health and Human Services, NIH seeks to improve our health by conducting and supporting research into the causes, diagnosis, prevention, and cure of human diseases; and other activities related to the nature and behavior of living systems with respect to enhancing health, lengthening life, and reducing illness and disability. |
|
No-Wrong-Door |
NWD |
A policy or system of policies that expands the number of entry points by which people can gain access to health or social benefits to which they may be entitled. |
|
Office of the National Coordinator for Health Information Technology |
ONC |
Part of the U.S. Department of Health and Human Services, ONC supports the adoption of health information technology and the promotion of nationwide health information exchange to improve healthcare. |
|
Parallel risk |
Designing contracts in ways that hold service providers with disparate funding streams financially accountable for meeting similar performance goals. |
|
|
Patient and Family Advisory Council |
PFAC |
A council that meets regularly and consists of patients and family members who have received care at a healthcare organization and its administrators, clinicians, and staff. Ideally, at least 50% of the council is patient and family advisors reflecting diversity of community served. This approach helps to promote a culture of patient- and family-centered care in the organization and enhance the delivery of high quality and safe care. |
|
Risk stratification |
The process of categorizing patients into tiers depending on the severity of their health-related needs and deploying resources accordingly. |
|
|
Scope of practice laws |
SoP |
State laws that authorize other qualified medical professionals, like nurse practitioners and physician assistants, to provide a limited set services that are traditionally provided by physicians. |
|
Shared decision making |
SDM |
A process in which clinicians and patients work together to make decisions and select tests, treatments and care plans based on clinical evidence that balances risks and expected outcomes with patient preferences and values. |
|
Social determinants of health |
SDoH |
The conditions in which people are born, grow, live, work and age that ultimately impact their health. |
|
Telemedicine |
The remote delivery of healthcare services and clinical information using telecommunications technology. This includes a wide array of clinical services using internet, wireless, satellite and telephone media. |
|
|
Triple Aim |
A framework for optimizing health system performance; includes improving the health of the population; enhancing the patient experience of care (including quality, access, and reliability); and reducing, or at least controlling, the per capita cost of care. |
|
|
Value-Based Payment |
VBP |
Purchasing practices that reward high-value care through payment incentives to providers. These approaches hold providers accountable for the quality and cost of the healthcare services they provide. Approaches largely fall into two categories: (1) measuring and reporting comparative performance; and (2) paying providers differentially based on performance. |
|
Wellness, well-being |
As used in this report, refers to the fulfillment of health and social needs. |