State News
Georgia
Georgia has made limited progress in closing the coverage gap – a key component of making healthcare affordable for residents. In 2019, state lawmakers approved three Medicaid waivers for CMS approval, which would limit the expansion of Medicaid in the state. However, there are no other efforts to expand Medicaid fully. While there are no consumer protections against rising drug prices, lawmakers have discussed implementing a drug discount program for its residents.
A 2020 Commonwealth Fund report ranked Georgia as 46th overall on health system performance. Additionally, Georgia performance in addressing maternal and child health issues has declined in the past three years. In 2019, Georgia lawmakers passed a bill that revamped Certificate of Needs laws in the state, to ease restrictions on hospital businesses. Like most states, Georgia has done little to address high healthcare prices or to tackling the spending associated unnecessary and low-value healthcare. Georgia has an all-payer claims database (APCD) in process. The state passed legislation in 2020 laying the groundwork for the creation of an APCD by Jan. 1, 2023.
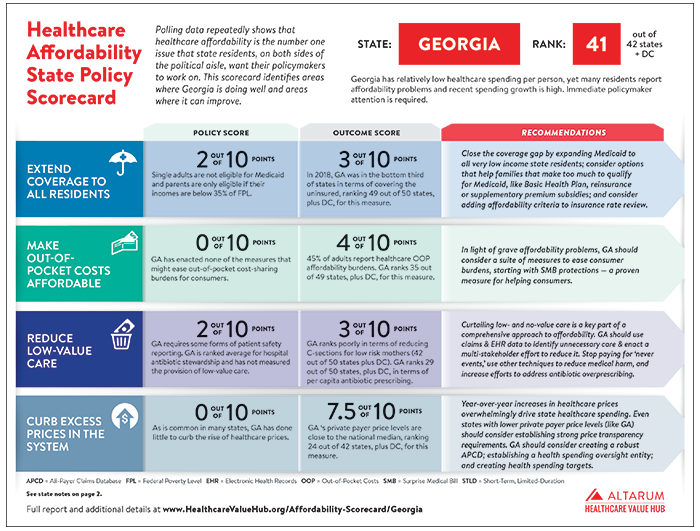
Georgia ranked 47 out of 47 states plus DC, with a score of 23.9 out of 80 possible points in the Hub's 2021 Healthcare Affordability State Policy Scorecard.
Georgia Requires Cost-Sharing Parity for Breast Cancer Exams and Increases Rural Hospital Tax Credit Cap
Georgia has passed legislation requiring insurance plans that cover diagnostic examinations for breast cancer to treat cost-sharing requirements the same as annual mammograms, according to AllOnGeorgia. The law is intended to increase access to life-savings health exams and increase the likelihood of early detection of breast cancer. In the same session, Georgia also passed HB 1041, which raises the cap on income tax credits for contributions to rural hospitals to $75 million per year in order to improve the financial solvency of the rural hospitals.
Georgia Passes Mental Health Reform Legislation
Georgia Governor Brian Kemp signed into law a bill intended to pressure private insurers to improve coverage for mental health conditions, according to an AP article in The Journal Record. The new law asks private insurers to follow established federal requirements to provide the same level of benefits for mental health disorders as they do for physical illness and requires insurers to submit data to the state about their compliance.
Georgia Patients Stranded Out of Network Following Severed Plan Contracts
After Wellstar Health System and UnitedHealthcare insurance did not agree on a new contract, Georgia resident Shelly Azzopardi was left without clear coverage for newly out-of-network follow-up services, according to Georgia Health News. Health care consultants and industry officials say an increasing number of contracts end without a deal, and even when they are resolved, they pressure thousands of patients to choose between higher out-of-pocket costs or leaving a trusted physician or hospital network. A similar dispute is looming involving Anthem Blue Cross and Blue Shield. This trend becomes more pressing as healthcare systems acquire additional hospitals and physician practices, effectively increasing the stakes of negotiation, and with it, the potential for patients to be left out of network if deals collapse.
Survey Finds Most Georgians Struggling to Afford Healthcare
70 percent of Georgia adults reported having burdensome healthcare costs in the last year and 80 percent are worried about being able to afford healthcare in the future, according to The Current. Specifically, 58 percent of adults encountered cost-related barriers to getting needed care, including skipping doses of medication and foregoing care altogether. Results were drawn from the Altarum Healthcare Value Hub's CHESS survey.
Insurers are Restoring Deductibles and Co-Pays for COVID, Leaving Patients with Big Bills
At the beginning of the coronavirus pandemic, insurers announced that they would cover all of the costs for COVID-19 treatment, but now, most insurers have reinstated co-pays and deductibles for COVID-19 patients, reports The Washington Post. Jamie Azar, who was hospitalized with COVID-19 in July, is facing thousands of dollars in co-pays, deductibles and out-of-network charges for her hospital and rehab stays for her treatment, with potentially thousands of dollars more in uncovered expenses as her recovery continues. The financial burden of COVID-19 is falling unevenly on patients across the country: health plan coverage varies widely across states, with only two states (Vermont and New Mexico) mandating complete insurer coverage of treatment. Azar—whose insurer reinstated patient cost-sharing on Jan. 31—now joins millions of other Americans with serious illnesses who face uncertain, confusing and expensive medical billing and insurance practices.
Clearer Path for Georgia Children to Receive Medicaid Passes General Assembly
The Georgia General Assembly unanimously passed a bill that would automatically enroll children who receive food stamps into Georgia’s Medicaid program, according to Northwest Georgia News. An estimated 60,000 Medicaid-eligible children will gain healthcare coverage through an automatic enrollment process that eliminates bureaucratic paperwork. Once the bill is signed by the governor, it will need approval from the federal government.
Federal Government Approves Georgia's State Relief and Empowerment Waiver
Georgia’s Section 1332 State Relief and Empowerment waiver has been approved, announced the Centers for Medicare & Medicaid Services (CMS). Beginning in plan year 2022, Georgia will implement a reinsurance program that is expected to reduce annual premiums for individuals by an average of 10 percent by covering some insurance costs once claims reach a certain amount. Beginning in plan year 2023, Georgia will transition the individual insurance market from a federally facilitated exchange to a private sector platform called the Georgia Access Model. The Georgia Access Model will serve as a one-stop shop that enables consumers to compare and enroll in plans offered by health insurance companies, web brokers and traditional agents and brokers. The state anticipates that the reinsurance program and the Georgia Access Model will increase health insurance affordability and enrollment.
Race and COVID-19: Stark Disparities in Rural Georgia
Of the ten counties nationally with the highest death rates from COVID-19, five are in Georgia, reports Georgia Health News. Hancock County is first on the list, with a COVID-19 death rate of 45.7 per 10,000 residents and a population where 3 in 4 residents are people of color. These counties are located in rural areas and have high levels of poverty and chronic disease, high uninsured rates, more older residents and large proportions of racial and ethnic minority groups. They also have a long history of systemic racism, which has served as a pre-existing condition for high COVID-19 death rates. Morehouse School of Medicine, an Atlanta school, is using a $40 million federal grant to implement an initiative to fight COVID-19 in minority rural communities.
Federal Government Approves Innovative State-Led Health Reform to Expand and Strengthen Coverage for Georgia Residents
Georgia’s new Medicaid Section 1115 demonstration program, “Pathways to Coverage,” has been approved, the Centers for Medicare & Medicaid Services (CMS) announced. This program will allow working-age Georgia residents (ages 19-64) who are otherwise ineligible for Medicaid to opt into Medicaid coverage by participating in qualifying activities, such as working 80 hours a month. The program applies to individuals with incomes less than or equal to 100% of the federal poverty level (FPL). The state expects over 30,000 Georgia residents will receive Medicaid coverage during the first year of this demonstration program.
Black Death Rate From COVID-19 in Georgia Far Higher Across All Ages
Black people in Georgia are dying from COVID-19 by as much as 3-4 times the rate for white people across all age groups, according to a new analysis in the Augusta Chronicle. The disproportionate impact of COVID-19 on Black people likely stems from systemic inequities in employment, education and access to healthcare, as well as the higher prevalence of chronic diseases among minorities.
Hospitals in Georgia are Charging Insurers More Than Twice Medicare Rates
RAND Corporation’s recent study shows that hospitals in Georgia charged private companies nearly three times the amount they were paid by the Medicare program for the exact same services, reports Georgia Health News. The gap between reimbursement from Medicare and private insurers has widened between 2016 and 2018. Lower reimbursements from Medicare and Medicaid has likely caused hospitals to “cost shift” and charge privately insured patients a higher rate for the same services.
Health Policy Win: Georgia Advocates Pass a New Law Protecting Consumers from Surprise Medical Billing
A new Georgia law protects patients from surprise medical bills in an emergency or when they receive care at an in-network healthcare facility but are treated by an out-of-network provider (such as an anesthesiologist), according to Community Catalyst. Patients will pay no more than they would have if the care had been received in-network, and providers cannot bill a patient for any additional amount, Arnold Ventures reports. However, Georgia’s bill extends only to state-regulated health insurance plans and certain public plans (such as the state employee health plan).
Measure to Curb Surprise Billing in Georgia Clears General Assembly
Georgia has passed legislation to end the practice of balance billing, according to the Cherokee Tribune & Ledger-News. The new law requires insurers to cover emergency services a patient receives whether or not the provider participates in the patient’s insurance coverage network.
Budget Cuts for Mental Health, Disabilities Alarm Patient Advocates
Georgia’s recent budget plans have been overturned by the overwhelming financial burden of the COVID-19 pandemic. The state’s Department of Behavioral Health and Developmental Disabilities outlined $172 million in budget reductions for the upcoming fiscal year. The budget cuts are alarming to patient advocates as the coronavirus crisis has sparked new mental health stresses. A Kaiser Family Foundation poll found that 56 percent of Americans reported that anxiety or stress related to the pandemic has led to at least one negative mental health outcome.
Study: Clinical Outcomes of Adult Patients Hospitalized with COVID-19
A recent study of COVID-19 patients in Georgia (primarily metropolitan Atlanta) showed that 1 in 4 hospitalized patients had no recognized risk factors for severe COVID-19. Most patients identified as Black, and their clinical outcomes were similar to those of non-Black patients. In other words, though the frequency of invasive mechanical ventilation and fatality did not differ by race, Black patients were disproportionately represented among hospitalized patients, reflecting greater severity of COVID-19 among this population.
Legislation to Curb Surprise Big Hospital Bills Passes Georgia Senate
Legislation aimed at ending surprise bills for emergency hospital visits in Georgia under certain insurance plans passed unanimously out of the Georgia Senate. According to Marietta Daily Journal, Senate Bill 359 would prohibit hospitals from handing patients unexpectedly large bills for emergency procedures done by specialists who are outside that hospital’s coverage network.
New Report Sets Stage for Georgia’s Healthcare ‘Waiver’ Debate
A state sponsored report curated by Deloitte provides an environmental scan of current uninsured Georgians. This study focuses on the uninsured rate if Georgia does not expand Medicaid, according to AJC. Researchers found that 666,000 Georgians could benefit from Medicaid expansion, indicating that uninsured rates are higher than previous estimates. Additionally, this study provides recommendations on waivers that state agencies and policymakers could pursue to seek more federal funding for their Medicaid program.
Georgia Certificate of Need Bill Passed by General Assembly
Georgia law makers passed House Bill 186, which revamped the state's Certificate of Need laws. According to Atlanta News Now, the bill was enacted to ease the restrictions on hospital businesses, and will allow hospitals to provide services to all patients that walk through their doors, without concern of cherry-picking by smaller healthcare start-ups. This bill will regulate smaller outpatient ambulatory and cancer centers at a county level.
State Task Force Eyes Healthcare Reform
Lt. Gov. Casey Cagle has tasked state Sen. Chuck Hufstetler, R-Rome, and four others to come up with a plan to bolster the state’s healthcare safety net system in light of federal intent to change the Affordable Care Act, according to Rome News-Tribune. Hufstetler views this as an opportunity to establish a program that could be used as a national model, where preventative care is key to success in improving health or reducing costs.
Battle Heats Up on Surprise Billing in Georgia Hospitals
For the second year in a row the debate over how best to address so-called ‘surprise medical bills’ has led to the introduction of legislation to prevent them, according to the Atlanta Journal-Constitution. While hospitals and physician groups remain broadly opposed to the measures, pressure from constituents has led multiple state representatives to press the issue in the legislature’s current session.
Patient-Centered Healthcare Program Proving Successful
Primary care physicians have been participating in Blue Cross Blue Shield of Georgia’s value-based, patient-centered program for three years and have delivered significant successes, according to SavannahNow. BCBS of Georgia’s data identified a 2 percent higher rate of care for diabetic patients, a 3.5-percent better rate of cervical and breast cancer screenings, and a 4.5-percent increase in patients taking their cholesterol, blood pressure and diabetes medications as prescribed.
Georgia Health Insurance Options are Bleak
Consumers shopping on the exchange for health insurance will face a myriad of challenges this year, according to the National Federation of Independent Business. Choice of providers has decreased from nine last year to five. Further, insurers have dramatically increased rates, the most staggering is Humana’s 67.5 percent rate hike.
New Program Helps Cut Costs in Crisp County
A Rural Hospital Stabilization Grant from the state of Georgia has funded a Mobile Integrated Healthcare Program at Crisp Regional Hospital that has reduced readmissions within 30 days of discharge from 35 to just 4, according to WALB News 10. The results stem from targeting “frequent flyers” -- people who frequently call 911 for non-emergencies -- and by providing unsolicited EMT visits to ensure these patients are taking care of themselves, such as taking their medication properly. The grant is set to expire in December 2016, but the hospital plans to continue the program.
Coordination Seen as Rural Health Remedy
A pilot program aimed at improving rural healthcare has provided insights into the problems caused by a lack of coordination and communication, according to the Valdosta Daily Times. The program, which received $6 million in funding and involves seven hospital systems, employs a hub-and-spoke model in which public health departments, nursing homes and other organizations collaborate and share information with hospitals, who serve as center of care.
Proceed with Caution: Proposed Health Insurance Mergers Could Harm Georgia Consumers
The proposed mergers between four of the nation’s five largest health insurers could lead to higher premiums and less choice for consumers, according to a report by the nonprofit Georgians for a Health Future. The report considers the impact the mergers would have on competition as well as potential policy remedies that would mitigate its impact should it eventually be approved.
A Review of Georgia Nonprofit Hospital Community Needs Assessments
A review of Community Health Needs Assessments that were performed by nonprofit hospitals in Georgia has offered insights into how hospitals are approaching their community benefit obligations under the Affordable Care Act. The report from Georgia Watch, a consumer advocacy group, reviewed 38 initial assessments that were conducted in 2012 and 2013.
Georgia Governor Signs Bipartisan Provider Directory Legislation
Georgia Governor Nathan Deal signed legislation aimed at improving the accuracy and usability of provider directories. The law, which was supported by consumer advocate organizations, will require health plans to maintain up-to-date provider directories for their plan participants.
Legislature OKs Tax Credits for Donations to Rural Healthcare Organizations
The General Assembly passed a bill that would allow an individual or corporation to receive a state tax credit for donating money to a rural health care organization, according to Georgia Health News. The rural health donation language was tacked on to Senate Bill 258, which dealt with general tax assessments.
More Georgia Hospital Mergers Loom
Merger talks are heating up in metro Atlanta, with Northside Hospital and Gwinnett Medical Center beginning talks to merge operations, according to Georgia Health News. The merger talks follow the recent aggressive moves of Marietta-based WellStar Health System. WellStar has begun talks to buy Tenet Healthcare’s five hospitals in metro Atlanta after earlier abandoning a proposed deal with Emory Healthcare. WellStar also has a proposed deal in place to acquire West Georgia Health.
Georgia hospital to pay $20 million to settle short-stay overbilling allegations
Modern Healthcare: The Medical Center of Central Georgia agreed to pay the federal government $20 million to settle allegations that it improperly billed short-stay admissions as inpatient rather than outpatient visits.
Report: State Lags in Public Health Spending
A report released in April by Trust for America's Health found that Georgia ranks 37th among states in per capita spending on public health. Georgia has a heavy disease burden, including high rates of HIV, hypertension, diabetes, tuberculosis and low-birth weight babies. The state also has large percentages of people living in poverty and without health insurance. The report said federal funding for public health has remained relatively flat for years.
Wellness Now the Watchword at Many Workplaces
Georgia Health News: Wellness programs could potentially help lower costs for employers however there is still controversy surrounding their implementation. In Georgia, many workplaces are turning to programs that stress nutrition and exercise as a means to the number of employees with diabetes.
Georgia Insurers, Doctors Partner to Improve Patient Care, Cut Costs
The Atlanta Journal-Constitution: A growing number of primary care providers in Georgia are partnering with insurers, hospitals and specialists to improve patient health outcomes by better coordinating care. Launched in 2013, this Blue Cross program is experimenting with paying doctors based on how patients fare rather than the traditional model of reimbursing for every service, test and office visit. Called Enhanced Personal Healthcare, the program has nearly 1,000 providers participating.
Rural Hospital Stabilization Committee Final Report
The Georgia Rural Hospital Stabilization Committee released a final report recommending including the establishment of a four-site pilot program, based on an integrated “hub and spoke” model, to relieve cost pressures on emergency departments and ensure that the best, most efficient treatment is received by patients. The committee also recommended increased support for telemedicine for rural hospitals.