The Consumer Benefits of Patient Shared Decision Making
From patient-centered medical homes to consumer-directed health plans, changes in the delivery, financing and organization of healthcare are increasingly touted as consumer- or patient-centered. Still, today’s health system is far from reflecting consumers’ true needs and preferences.1
Patient shared decision making (PSDM) is a technique to incorporate patients’ needs and preferences into their individual treatment plans. PSDM goes beyond traditional informed consent in healthcare—it is an interpersonal, interdependent process in which healthcare providers and patients collaborate to make decisions about the care that patients receive. Shared decision making not only reflects medical evidence and providers’ clinical expertise, but also the unique preferences and values of patients and their families.
Given that this strategy has considerable advantages and few disadvantages, it is used far too infrequently. Policymakers, payers and health systems should advocate for patient shared decision making to be the standard of care for all clinical encounters that have more than one medically appropriate path forward.
This report describes patient shared decision making and reviews the evidence supporting its use. Existing challenges and strategies to expand the use of PSDM are also discussed.
What is Patient Shared Decision Making?
Shared decision making is a key component of patient-centered health care. It is a process whereby clinicians and patients work together to make treatment decisions and select tests, care plans and supportive services in a way that balances clinical evidence on risks and expected outcomes, with patient preferences and values.2
There are three essential elements that must be present for shared decision making to occur:
- Both the healthcare provider and the patient must recognize and acknowledge that a decision is required.
- Both must understand the risks and benefits of each option.
- Decisions must take into account both the provider’s guidance and the patient’s values and preferences.3
For some medical conditions, there is only a single treatment path in which patient preferences play a minor role. These situations might include a fractured hip repair, surgery for acute appendicitis or antibiotics for bacterial meningitis.4 However, most diagnoses have more than one medically appropriate path forward, with different potential outcomes and side effects.5 Examples of these circumstances include treatments for early-stage cancer, primary prevention of coronary heart disease and the use of genetic and blood screening tests.
When more than one medical treatment exists, clinicians can facilitate shared decision making by encouraging patients to voice their concerns and priorities. They can also offer decision aids to increase patient awareness and understanding of the various treatment options and possible outcomes.
Patient Decision Aids
A well-designed patient decision aid provides actionable information on the risks, benefits and burdens of treatment options, and helps patients identify and communicate their preferences.6 These aids can be web-based, printed materials or educational videos that help patients understand relevant clinical evidence, develop informed preferences and communicate them to their providers.7 A 2011 study showed that decision aids perform better than traditional, non-shared decision making care interventions in clinical settings, and significantly improved patients’ knowledge of their conditions and treatment options.8
But shared decision making is more than just the use of decision aids. It requires meaningful clinician-patient engagement.
Barriers to Effective Patient-Physician Communication
Patient shared decision making requires open and respectful communication between the patient and physician, but myriad factors can undermine this type of exchange. For example, both patient and physician may approach the conversation with pre-conceived notions that hinder the shared decision-making process.
Some patients distrust or feel uncomfortable discussing health concerns with doctors who they cannot relate to on a personal level.9 For example, elderly patients, patients who speak English as a second language and those with lower literacy levels may feel less engaged in the decision-making process and have less confidence navigating the healthcare system.10 Other patients might come from cultural backgrounds that lack a tradition of individuals making autonomous decisions, thus making it difficult for them to engage with their provider.
Physicians can also unwittingly introduce barriers. Many doctors believe that they are good at identifying patient preferences, but there are enormous gaps between what patients want and what doctors think they want.11 For example, a physician may believe that a patient with prostate cancer’s priority is to remove the cancer, while the patient’s priority may be to maintain the best possible quality of life. The misdiagnosis of patient preferences thus becomes a deterrent to delivering patient-centered care.12 Moreover, doctors may unknowingly hold biases toward patients who they feel are not able to understand complex medical information.13
Ineffective patient-physician communication can also be attributed to the lack of emphasis on communication skills during medical training. Most communication training takes place during the preclinical years of medical school in the form of lectures and role plays with patients. During clinical rotations, students have direct encounters with patients, but little attention is devoted to communication abilities compared to diagnostic skills.14 Similarly, strong communication skills are often not stressed in postgraduate medical training, leaving residents and practicing physicians to learn to communicate effectively on their own.
Evidence Around Shared Decision Making
The evidence around shared decision making is fairly strong. Shared decision making has been shown to result in treatment plans that better reflect patients’ goals; increase patient and physician satisfaction; improve patient-physician communication; have a positive effect on outcomes; and, sometimes reduce costs.
Patient and Physician Satisfaction
Having a forum to voice their preferences and understanding the risks and benefits associated with their decisions makes patients happier with the care they receive. One study found that patients who participated in shared decision making were more knowledgeable about their condition (compared to a control group) and, when given their treatment of choice, reported higher overall quality of life after six months.16 Additionally, these patients were far more likely to be satisfied with their treatment, with about 71 percent satisfied, compared to about 35 percent of patients who did not engage in PSDM.17 Patients who made informed decisions were also less likely to regret their treatment choices (about 5 percent, compared with 15 percent of patients in the control group).18
Shared decision making can also increase physician satisfaction as a result of feeling that they are supporting and listening to their patients while providing high-quality care.19
Improved Communication
Shared decision-making techniques can help patients establish trust with their providers and helps providers engage and better communicate with their patients. A 2013 study assessed the relationship between African American patients and their providers using conversation guides to lead patient-physician conversations. Qualitative interview data showed patients’ trust in physicians increased after using the conversation guides.20 Researchers further noted that, while PSDM can increase trust, using other specific techniques in combination with PSDM was particularly effective. Specifically, mistrust of physicians among African Americans with diabetes may partially be addressed through patient education efforts and physician training in interpersonal skills and cultural competence. Other research shows that, when physicians understand cultural and other personal factors of a patient, the patient is more inclined to trust the provider with their care.21
Positive patient-provider relationships are not just part of good bedside manner; perceived respect has a strong correlation with whether patients trust doctors to be accurate and whether they adhere to their medications. Thus, strong relationships should be considered a medical priority and should be encouraged through training, education and, potentially, compensation changes.22
Improved Outcomes
Research reveals that patients who are empowered to make healthcare decisions that reflect their personal preferences often report feeling more engaged in their healthcare and experience better health outcomes, like decreased anxiety, quicker recovery and increased compliance with treatment regimens.23
A 2017 review of 105 studies showed that use of decision aids reduced the number of patients that were passive in their treatment and increased patient adherence to recommended therapies.24 Patients also had increased knowledge, more accurate perception of risk and reduced internal conflict about healthcare decisions.
Reduced Costs
Preference-sensitive conditions, such as treatments for joint arthritis, back pain and early stage prostate cancer,25 are medical conditions in which the clinical evidence does not clearly support one treatment option, and the appropriate course of treatment depends on the values or preferences of the patient.26 People who are fully informed about the risks and benefits of treatments and screening for preference-sensitive conditionstend to choose less-invasive, less-costly interventions and are happier with their decisions.27
Concerns have been raised that offering patients more options may increase costs.28 To date, the cost of implementing shared decision making has been studied in only a limited number of practice settings and typically in relatively small patient populations.29
One study compared the cost of care for an uncomplicated menorrhagia among patients that received a decision aid, patients that received a decision aid followed by a nurse’s coaching to elicit patient preferences, and a control group. The analysis found that a decision aid, either implemented alone or with coaching, had lower mean costs ($2,026 and $1,566 respectively) than the control group ($2,751).30
In addition, a 2012 study showed that providing decision aids to patients eligible for hip and knee replacements substantially reduced surgery rates and costs—with up to 38 percent fewer surgeries and a 12 to 21 percent savings over six months.31 Across a few studies, as many as 20 percent of patients who participated in shared decision making chose less invasive surgical options and more conservative treatment than patients who did not use decision aids.32
Nevertheless, more study is needed to understand the net costs of implementing shared decision making in a variety of treatment scenarios.
Challenges to Expanding the Use of Shared Decision Making
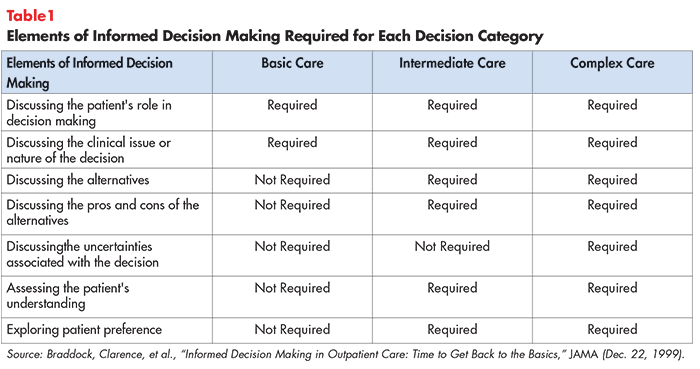
Despite the potential benefits, shared decision making has not been widely implemented in clinical practice. Many clinicians find PSDM difficult to accomplish, and most healthcare systems do not view this approach as the standard of care. In a study of more than 1,000 office visits in which more than 3,500 medical decisions were made, less than 10 percent of decisions met the minimum standards for shared decision making (see Table 1 for elements of informed decision making).33
Another study showed that only 41 percent of Medicare patients believed that their treatment reflected their preference for palliative care over more aggressive interventions.34 Additionally, patients report frustration and dissatisfaction because they do not feel like they have adequate (if any) input into clinicians’ decisions that affect their health,35 including not knowing enough about their treatment options to make informed decisions.
Challenges to expanding the use of shared decision making include:
- Belief that PSDM is not appropriate or necessary for provider's specialty;
- decision aid shortcomings;
- provider time constraints;
- provider reimbursement not aligned with PSDM;
- provider training; and
- malpractice liability
Belief that PSDM is Not Appropriate or Necessary for Provider’s Specialty
A systematic review of barriers to PSDM found that many physicians perceive PSDM to be inappropriate for their patients or clinical specialty.36 Health professionals’ tendency to decide which patients will prefer or benefit from shared decision making is concerning because physicians might misjudge patients’ desire for active involvement in their treatment.
A 2016 study focused on ulcerative colitis patients who faced two treatment options with significant, life-altering side effects.37 Researchers hypothesized that patients would be conflicted about the side effects of the treatments, but a patient preference analysis revealed otherwise. Patients were fundamentally concerned with the progression of their ulcerative colitis.38 These results demonstrated that doctors do not always know what matters most to patients.
Other common barriers include the perception that shared decision making is already occuring, that patients don’t want it, that it is ineffective39 and that many patients cannot understand their options.40 According to a 2014 Altarum survey, 37 percent of physicians believe that patients want the doctor to make the decisions regarding their medical treatment (with minimal input from the patient), but only 7 percent of patients selected this as the role they wanted doctors to have.41 Nearly 9 in 10 consumers say if their doctor provides them with material when diagnosed with a health condition, they read it as soon as possible.42
Decision Aid Shortcomings
The use of decision aids is a key component of PSDM. Providers have reported that decision aids increase cohesion among team members (including patients) and facilitates patient education in both clinical and telemedicine settings.43 But decision aids are only effective if they are accurate and present the information in ways that patients with varying literacy levels, language and cultural backgrounds can understand. For example, some Latina patients were more responsive to a patient decision aid designed as a short soap opera that tells the story of a person in a similar situation.44
Another challenge for patient decision aids is to keep pace with rapidly changing developments, including new treatment alternatives and new information concerning treatment efficacy and complications. Although the International Patient Decision Aid Standards (IPDAS) Collaboration has created a standard checklist45 for high-quality decision aids, there is currently no national body responsible for certifying decision aids that adhere to the checklist. Certification helps providers, patients and payers evaluate the quality of decision aids and is needed to ensure that decision aids are unbiased, comprehensive, accurate and up-to-date.46 Barriers to certification include the cost and laborious process of certifying materials.
Provider Time Constraints
Time constraints remain the most frequently cited barrier to implementing shared decision making in clinical practice.47 Specifically, time pressures make it difficult to listen to patients, address their needs and emotional concerns and help them make decisions that are consistent with their values and preferences.
PSDM’s impact on consultation length is unclear, as studies have shown both increases and decreases in consultation length after patients have viewed a decision aid.48 More research is needed to understand the impact of shared decision making on providers’ work schedules.
Provider Reimbursement is Not Aligned with PSDM
Another barrier to integrating PSDM into common practice is that fee-for-service payment systems do not typically reimburse clinicians for time spent engaging with patients in shared decision making.49
There has been considerable debate over whether to reimburse providers for participating in PSDM or if PSDM should be part of routine care that is not reimbursed separately. As noted above, PSDM’s impact on consultation length is unclear, leaving the implications for reimbursement ambiguous.50 Also debated is the type of providers that should engage with the patient (specialist, primary care or nurse) in PSDM.
Regardless of reimbursement, health systems have struggled to supply hospitals and other care settings with sufficient resources (such as decision aids or education campaigns for patients and providers) to incorporate PSDM into the care process.
Provider Training
PSDM training has has been shown to increase provider’s confidence and knowledge, enabling them to facilitate PSDM more easily.51 There are currently 83 training programs in the United States but, due to providers’ and health systems’ attitudes towards PSDM, these programs are not widely used.52
Malpractice Liability
Another challenge that is particularly concerning to hospitals and providers is medical malpractice. Patients may be more likely to sue if they choose not to have procedures or screening through PSDM, but develop a more serious condition later on.53
Concerns about medical malpractice are less common among providers than concerns about time constraints and applicability of PSDM to clinical situations. One study found that using a decision aid in conjunction with PSDM offered protection for physicians against a malpractice ruling in a mock trial.54 Although the impact of PSDM on malpractice lawsuits is ambiguous, it remains a concern.
Best Practice Strategies to Implement PSDM
The Patient’s Role
Providers must recognize that patient preferences vary with respect to being actively involved in their care.
The vast majority of Americans (86%) trust their doctor.55 For some, this results in a reluctance to take a more active role in their care.56 However, many patients express dissatisfaction with their physician because they do not feel that they have had adequate input into their providers’ decisions about their health.57
One factor that contributes to this problem is that patients often do not know enough about their treatment options to make informed decisions. Most consumers (95%) believe it is important that doctors tell them about the results of medical research when making treatment decisions.58
As described above, patient decision aids are a strategy to guide the patient in the development of their care plan. To further open lines of communication, researchers recommend encouraging patients to ask their providers three or four general questions when discussing treatment options. These include: “What are my options?” “What are the benefits and harms?” “How likely are negative effects?” and “What will happen if I do nothing?” This strategy alone has been shown to improve both the consultation process and patient outcomes.59
Patients will continue to have different preferences when it comes to being involved in their care. Nonetheless, there is strong evidence that more engaged patients have better health outcomes and care experiences.60 Thus, PSDM should guide patients to the extent to which they are comfortable.
The Provider’s Role
Assessing a patient’s personal preferences should begin with determining how large of a role the patient wants to play in his or her care. Clinicians should assess these values at the start of the care process and design their treatment approach accordingly.61 They must uncover the motivating factors that drive a patient’s decision rather than make assumptions.
Using decision aids can help clinicians more efficiently elicit patients’ preferences. Some providers will need to approach the clinical interaction in a new way, giving up their authoritative role and becoming more effective coaches or partners. The ability to ask, “What matters to you?” as well as “What is the matter?” can go a long way in beginning a fruitful dialogue.62
Electronic medical records can provide informal training by identifying patients who will be facing a medical decision and reminding providers to offer patients decision aids and engage in a PSDM conversation.63
Three main motivators help providers implement shared decision making in clinical practice: (1) health professionals’ internal motivation, (2) the perception that practicing shared decision making will lead to improved patient outcomes and (3) the perception that practicing shared decision making will lead to improved healthcare processes.64 These motivators may need to be leveraged to shift providers’ attitudes towards PSDM.
The Caregiver's Role
As with many aspects of patient care, involving family members and caregivers is important. Patients lean on their loved ones during times of uncertainty and poor health.
Involving family members in the care decision-making process is a key strategy to supporting high-quality patient care and delivering a positive experience. Strategies to engage families and caregivers in shared decision making are similar to those that strive to engage individual patients. Providers need to offer ample information to support the decision at hand and embrace a patient- and family centered approach. Clinicians must also take into account the patient’s preferences for family involvement. In some cases, patients may not want high levels of family engagement.
Conclusion
Given the fact that PSDM has considerable advantages and few disadvantages, it is used far too infrequently. As noted above, in a study of more than 1,000 office visits involving more than 3,500 medical decisions, less than 10 percent of decisions met the minimum standards for shared decision making.
In the effort to create a high quality, patient-centered healthcare system, policymakers, payers and healthcare facilities should make shared decision making the standard of care for all clinical encounters with more than one medically appropriate path forward.
Success in this endeavor will require proactively addressing the barriers described in this research brief, such as lack of physician buy-in, lack of time, lack of reimbursement, poor integration into clinical workflows and a scarcity of information designed for patient use. Training programs, educational materials and inclusive dialogue can help providers and patients make PSDM a routine component of patient-centered care.
Notes
1. Ditre, Joe, Consumer-Centric Healthcare: Rhetoric vs. Reality, Healthcare Value Hub, Research Brief No. 18 (May 2017).
2. Patient Advocate Foundation, The Roadmap to Consumer Clarity in Health Care Decision Making (2017).
3. Légaré, France, and Holly O. Witteman, “Shared Decision Making: Examining Key Elements and Barriers to Adoption into Routine Clinical Practice,” Health Affairs, Vol. 32, No. 2 (February 2013).
4. Barry, Michael J., and Susan Edgman-Levitan, “Shared Decision Making—The Pinnacle of Patient-Centered Care,” NEJM, Vol. 366 (March 2012).
5. Ibid.
6. National Quality Forum, Shared Decision Making: A Standard of Care for All Patients, Washington, D.C. (2017).
7. Barry (March 2012).
8. Stacey, Dawn, et al., “Decision Aids for People Facing Health Treatment or Screening Decisions,” Cochrane Database (October 2011).
9. Ibid.
10. Ernst, Alexandra, et al., Shared Decision Making: Engaging Patients to Improve Health Care, Families USA, Washington D.C. (May 2013).
11. Ha, Jennifer F., et al., “Doctor-Patient Communication: A Review,” The Ocshner Journal (2010); Ditre (May 2017).
12. Légaré (February 2013).
13. Elwyn, Glyn, et al., “Shared Decision Making: A Model for Clinical Practice,” Journal of General Internal Medicine, Vol. 27, No. 10 (May 2012).
14. Choudhary, Anjali, and Vineeta Gupta, “Teaching Communications Skills to Medical Students: Introducing the Fine Art of Medical Practice,” International Journal of Applied and Basic Medical Research (August 2015).
15. Berman, Amy, “Living Life in My Own Way—And Dying That Way As Well,” Health Affairs (April 2012).
16. “Shared Decision Making Leads to Better patient Outcomes, Higher Satisfaction Rates,” News Medical Net. https://www.news-medical.net/news/20170314/Shared-decision-making-leads-to-better-patient-outcomes-higher-satisfaction-rates.aspx (accessed March 17, 2018) and https://www.aaos.org/AAOSNow/2015/Jan/managing/managing2/?ssopc=1
17. Ibid.
18. Ibid.
19. Dobler, Claudia, et al, “Can Shared Decision Making Improve Physician Well-Being and Reduce Burn-Out?” Cureus (August 2017).
20. Peek, Monica, et al., Patient Trust in Physicians and Shared-Decision Making Among African-Americans with Diabetes, National Institutes of Health (October 2012).
21. Légaré (February 2013).
22. Altarum Institute and Oliver Wyman, Right Place, Right Time Improving Access to Health Care Information For Vulnerable Patients—Consumer Perspectives (January 2017).
23. Agency for Healthcare Research and Quality, The CAHPS Ambulatory Care Improvement Guide: Strategy 6I: Shared Decision Making, Rockville, MD (2017).
24. Stacey, Dawn, et al., “Decision Aids for People Facing Health Treatment or Screening Decisions,” Cochrane Database (April 2017).
25. Veroff, David, et al., “Enhanced Support for Shared Decision Making Reduced Costs of Care for Patients with Preference-Sensitive Conditions,” Health Affairs, Vol 32 No. 2 (February 2013).
26. Centers for Medicare and Medicaid Services, Beneficiary Engagement and Incentives Models: Shared Decision Making Model, https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-12-08-2.html (accessed March 14, 2018).
27. O’Malley, Ann S., et al., Policy Options to Encourage Patient-Physician Shared Decision Making, National Institute for Health Care Reform, Washington, D.C. (September 2011).
28. Shafir, Adi, and Jill Rosenthal, Shared Decision Making: Advancing Patient-Centered Care Through State and Federal Implementation, National Academy for State Health Policy, Washington, D.C. (March 2012).
29. Ibid.
30. Kennedy, Andrew, et al., “Effects of Decision Aids for Menorrhagia on Treatment Choices, Health Outcomes, and Costs,” JAMA, Vol. 288, No. 21 (January 2003).
31. Arterburn, D., et al., “Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs,” Health Affairs, (September 2012).
32. Lee, Emily O., and Ezekiel J. Emmanuel, “Shared Decision Making to Improve Care and Reduce Costs,” NEJM, Vol. 368 (January 2013).
33. Braddock, Clarence H., et al., “Informed Decision Making in Outpatient Practice,” JAMA Network (December 1999).
34. Ibid.
35. Agency for Healthcare Research and Quality, The CAHPS Ambulatory Care Improvement Guide, Rockville, MD (December 2017).
36. Légaré, France, et al., “Barriers and Facilitators to Implementing Shared Decision Making in Clinical Practice: Update of a Systematic Review of Health Professionals’ Perceptions,” Patient Education and Counseling, Vol. 73, No. 3 (August 2008).
37. Heath, Sarah, “How to Include Patient Preferences in Shared decision making,” Patient Engagement HIT (Aug. 1, 2016).
39. Légaré (August 2008).
40. Lynch, Wendy, Kristin Perosino and Michael Slover, Altarum Institute Survey of Consumer Healthcare Options, Altarum (Fall 2013).
41. Ibid.
42. Harris Poll, Consumer Attitudes About Health Study (March 30, 2016).
43. Griffith, Michelle, et al., “A Shared Decision-Making Approach to Telemedicine: Engaging Rural Patient in Glycemic Management,” Journal of Clinical Medicine, Vol. 5 No. 11 (November 2016).
44. Ernst (May 2013).
45. International Patient Decision Aid Standards, Criteria for Judging the Quality of Patient Decision Aids (2005).
46. Shafir and Rosenthal (March 2012).
47. Légaré (August 2008).
49. Hibbard, Judith and Helen Gilburt, Supporting People To Manage Their Health: An Introduction To Patient Activation, The King’s Fund (May 2014).
50. Ibid.
51. Ibid.
52. Diouf, Ndeye, et al., “Training Health Professionals in Shared Decision Making: Update of an international Environmental Scan,” Science Direct, Vol. 99, No. 11 (November 2016).
53. Durand, Marie-Anne, et al., “Can Shared Decision Making Reduce Medical Malpractice Litigation? A Systematic Review,” BMC Health Services Research (April 2015).
54. Barry, Michael J., et al., “Reactions of Potential Jurors to a Hypothetical Malpractice Suit Alleging Failure to Perform a Prostate-Specific Antigen Test,” Journal of Law, Medicine, and Ethics (June 2, 2008).
55. Healthcare Value Hub, Consumer-Centric Healthcare: Opting for and Choosing Among Treatments, Easy Explainer No. 10 (2017).
56. Ibid.
57. Agency for Healthcare Research and Quality, The CAHPS Ambulatory Care Improvement Guide, Rockville, MD (December 2017).
58. Healthcare Value Hub, Consumer-Centric Healthcare: Opting for and Choosing Among Treatments, Easy Explainer No. 10 (December 2017).
59. Ibid.
60. Hibbard, Judith H., and Jessica Greene, “What the Evidence Shows about Patient Activation: Better Health Outcomes and Care Experiences; Fewer Data on Costs,” Health Affairs, Vol. 32, No. 2 (February 2013).
61. The Agency for Healthcare Research and Quality developed the SHARE Approach and other tools as a resource for providers: https://www.ahrq.gov/professionals/education/curriculum-tools/shareddecisionmaking/index.html
62. Barry (March 2012).
63. Shafir and Rosenthal (March 2012).
64. Ibid.