Consumer-Centric Healthcare: Advocating for Health System Improvements
Healthcare is increasingly touted as consumer- or patient-centered. Research is beginning to show that revealing and catering to consumer preferences can lead to better outcomes, more efficient spending and higher patient satisfaction. But our health system too often fails to provide what consumers really want and need.
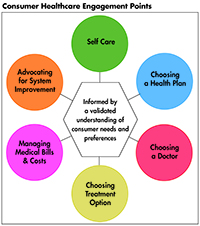
This Easy Explainer describes one of six consumer healthcare engagement points explored in the Hub’s Research Brief No. 18, Consumer-Centric Healthcare: Rhetoric vs. Reality, which outlines how these failings could be addressed and encourages a discussion of how to elevate, support and validate the consumer’s voice.
What are Consumers’ Preferences and Needs?
Consumers are the ultimate payers of all health costs. Whether paying through reduced wages for employer sponsored insurance, taxes for public coverage, or out-of-pockets costs for direct care or coverage, consumer dollars are at stake. Yet, when it comes to policy matters and shaping the direction of the healthcare system for which they pay, consumers have relatively no voice, no power, and no seat at the table. In this context, it becomes clear that terms such as consumer-oriented, consumer-driven, and patient-centered were largely developed by others-whether well-intentioned or not-for consumers, but not with consumers.
Given the imbalance of power in our healthcare system, consumers need a place at the table where decisions are being made about them, their care and the prices they pay.
How Does the System Fail Consumers?
Corporate organizational and governmental regulatory policies often lack institutional mechanisms for consumers to provide input. And when these roles do exist, they almost always lack dedicated resources to support consumer participation and put consumers on a level playing field with other stakeholders.
To maximize consumer engagement while minimizing consumer burden, we need to look across both formal and informal means of ensuring the consumer perspective is included.
Informal pathways include leveraging feedback mechanisms and complaint systems, consumer surveys, real world observations and extrapolating from available data. But we rarely leverage or support these pathways. For example, the vast majority of consumers do not realize that they have a state insurance regulator who can address their insurance problems.1 Under these circumstances, we must extrapolate from consumer complaint data rather than rely upon it as a faithful representation of how consumers are faring in the healthcare marketplace.
We also see a failure to include consumers in hospital governance structures and legislative taskforces. Further, when these roles exist, consumer members are often under-supported by the absence of funds for transportation, for technical support, and other resources that would make them effective members.
As a result, individuals playing these roles are often outgunned and out resourced by the other stakeholders around the table.
How the System Can Better Meet Consumers’ Preferences and Needs?
It is clear that consumers need a place at the table where decisions are being made about the care they receive and the prices they pay. But they need to be supported in this role, with reimbursement for transportation, access to technical assistance and other resources to put them on a level playing field with the other, more powerful, stakeholders.
Emerging evidence suggests that consumer and patient engagement into health system organizational design and governance can be a pathway toward achieving the goals of better quality of care, greater cost efficiency, and improved population health.2
South Australia provides a good example of a government-supported consumer-engagement program,3 to recognize the value of the consumer voice and to provide consumers with a seat at the table. The regulatory framework4 for implementing the program states it will:
- ensure there are mechanisms in place to actively engage with consumers and the community in order to identify their needs, and also develop appropriate services;
- partner with consumers and the community in the planning, implementation and evaluation of its service;
- strengthen responsiveness to the differing perspectives and needs of a diverse range of consumers and community members;
- provide accessible engagement strategies that are acceptable to a broad range of consumers and the community developing a culturally responsive healthcare system;
- develop a culturally responsive healthcare system; and
- ensure the methods and practice of consumer engagement are guided by current best practice.
One of the program’s mechanisms for bringing the consumer voice into policy are “Health Policy Councils,” which the Minister for Health can establish “to undertake an advocacy role on behalf of the community, undertake consultancies with the community, and provide advice to the Minister and the Chief Executive in relation to health matters, among other functions.”5
In the U.S. we have local examples that we can replicate more vigorously. For example, there is a mandate in Massachusetts for hospitals to establish patient and family advisory councils.6 There are also health systems that build patient and family advisory councils into their operations.7
Similarly, government should develop create mechanisms for patients and caregivers to provide input and shape policy. For example, community health centers are required under the Public Health Service Act to have a consumer majority on their board of directors.
Notes
1. Surprise Medical Bills Survey: 2015 Nationally-Representative Online Survey, Consumer Reports (May 5, 2015).
2. Carman, Kristen, et al. (April 2016).
3. South Australian Public Health Act of 2011 (2011). See: https://www.legislation.sa.gov.au/lz/c/a/south%20australian%20public%20health%20act%202011/current/2011.21.un.pdf.
4. Directive: Compliance is Mandatory: A Framework for Active Partnership with Consumers and the Community, Government of South Australia-SA Health (Dec. 20, 2012).
5. Ibid
6. An Act To Promote Cost Containment, Transparency, And Efficiency In The Delivery Of Quality Health Care 188th General Court of the Commonwealth of Massachusetts. Session laws: Acts (2008): Chapter 35 (2008).
7. Johnson, Bev, et al., Partnering with Patients and Families to Design A Patient- and Family-Centered Health Care System, Institute for Family-Centered Care (April 2008).