High-Value Care: Strategies to Address Underuse
Policy and practice debates seeking to improve healthcare delivery and control health spending often focus on reducing the provision of low- or no-value care.1 Yet, research shows that Americans are only receiving 55 percent of recommended care, so the goal of reducing low-value care needs to be balanced with an emphasis on increasing the provision of high-value care.2
This research brief looks at high-value services we should provide more frequently if our country is to move to a high-value healthcare system. Specifically, this brief reviews circumstances where high-value care is under-consumed and the strategies that can ensure patients receive proper levels of care, including provider incentives and consumer nudges.
What is High-Value Care?
High-value healthcare services are those of proven value and with no significant tradeoffs. Moreover, the benefits of the services so far outweigh the risks that all patients with specific medical conditions should receive them.3 Simply put, these are services we should be doing more of.
High-value services are essential to, but distinct from, a high-value healthcare system where all incentives are aligned to create an environment where providers can give the best care possible, use resources efficiently and reduce health inequities.4
Several organizations have used a variety of methods to identify high-value services.To start, the Institutes of Medicine (IOM) noted in their 2010 Workshop Series Summary—The Healthcare Imperative: Lowering Costs and Improving Outcomes—that there are three levels of services to improve individual and population health:
- community-based prevention services, like counseling services in the community to help modify problematic and expensive health behaviors (e.g., smoking, unhealthy diet, physical activity, and alcohol abuse);
- primary and secondary level clinically-based prevention services like blood tests, nutrition counseling, or screenings for various diseases (primary prevention attempts to prevent disease from occurring—e.g., immunization—whereas secondary prevention attempts to minimize the effect of disease—e.g., through colorectal cancer screening);
- tertiary prevention attempts to slow the progression or reduce the disability caused by a disease. Targeting individuals with one or more chronic conditions, these services include services such as foot or eye exams for people with diabetes, or prescribing aspirin to patients who are hospitalized from coronary artery disease.5
The IOM report noted these services do not always result in net medical savings, highlighting the importance of including the value of improved health in cost-benefit calculations. For example, alcohol and tobacco use screenings have the potential for an annual net savings of nearly $1.5 billion when applied to the general U.S. population, whereas the use of secondary preventive services, such as mammograms and depression screenings, results in net medical costs of almost $2 billion.6
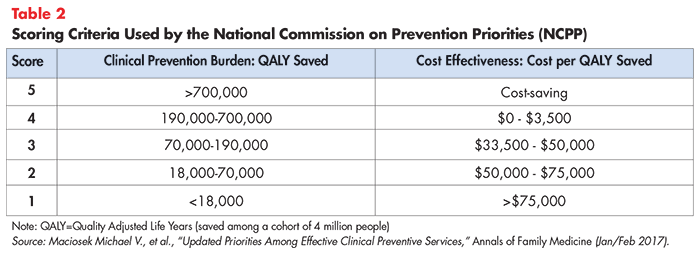
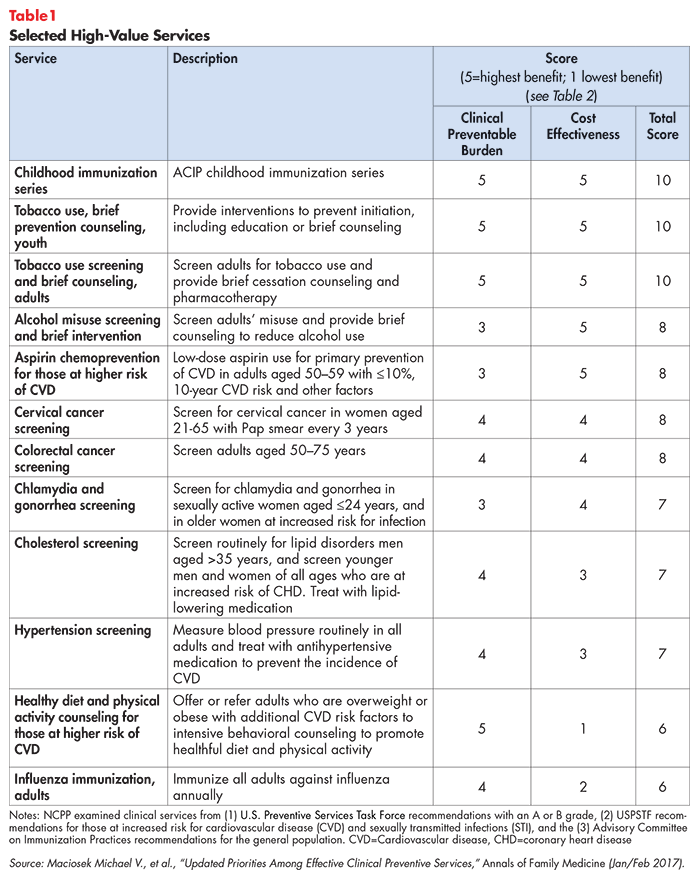
The Committee on Clinical Preventive Services Priorities and the National Commission on Prevention Priorities (NCPP) have identified both community-based prevention services, as well as primary and secondary clinical services that score well in terms of the health impact (termed “clinical preventable burden”) and cost effectiveness (see Table 1).7 Table 2 shows the quality-adjusted life years and savings criteria NCPP used to determine the scores for the high-value services listed in Table 1.
Preventive tertiary care is typically viewed as an excellent opportunity to lower spending while improving health since patients with chronic conditions typically have a high baseline use of expensive health services (like hospital care).8 Not only do these high-value tertiary services improve patient health, thus reducing spending on hospital stays, but the investments can produce indirect savings like reducing missed days at school or increasing worker productivity.9
Failures to Deliver High-Value Care
The IOM researchers and others have found that the United States fails to deliver high-value care at recommended levels.10 The IOM estimated more than $55 billion in savings each year by increasing the provision of primary, secondary and tertiary high value, prevention services. A more recent study found that only 8 percent of U.S. adults ages 35 and older had received all high priority, appropriate clinical preventive services recommended for them.11 Even worse, nearly 5 percent of adults did not receive any such services.
Moreover, racial and ethnic groups appear to be disproportionately slighted in their receipt of high-value care. For example, minorities often receive fewer preventative screenings than white patients, even controlling for insurance status, despite research showing that minorities are disproportionately affected by chronic conditions.12 Additionally, researchers from Harvard T.H. Chan School of Public Health and Brigham and Women’s Hospital discovered that overall receipt of high-value services like weight reduction counseling, aspirin use for coronary artery disease, statin use in diabetes and treatment for depression was lower among Medicaid patients compared to privately insured patients.13
Policies to Encourage Provision and Use of High-Value Care
Increasing the provision and use of high-value care can be accomplished by using several policy levers, including provider incentives and consumer nudges.
Create Strong Evidence-Based Practice Guidelines and Properly Disseminate Them
Providers need certainty when it comes to knowing what care to deliver. In general, practice guidelines can use a wide range of evidence standards. A 2008 review of 53 guidelines for cardiologists, involving more than 2,700 treatment recommendations, found that only 11 percent of guidelines were backed by strong evidence from multiple randomized clinical trials.14 Meanwhile, 48 percent of the recommendations were based on the personal opinions of experts in the field. Another study found that many practice guidelines were of uncertain relevance to patients in primary care.15 Physicians and patients are aware of the well documented disagreements across the American College of Obstetricians and Gynecologists, the American Cancer Society and the U.S. Preventive Services Task Force Services with respect to the recommended age to begin mammography screening for women.
The high-value care examples included in this brief have strong evidence with respect to the reduction of disease burden but increased funding for comparative-effectiveness could undoubtedly add more services to our list of high-value services.
Provider Financial Incentives
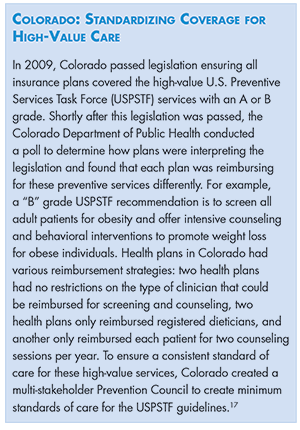
Provider payment reform is a key tool to accomplish many health system transformation goals. Typically, these reforms seek to move away from traditional fee-for-service reimbursements because it incentivizes volume over value. But to incentivize discrete high-value services like flu vaccinations or high-value screening services, payers and policymakers may want to use fee-for-service payments specifically to incentivize greater volumes for these services (see Colorado box).16
Pay-for-performance, also referred to as value-based purchasing, are payment approaches intended to improve provider quality and reduce costs.18 Pay-for-performance (PFP) programs incentivize providers to meet or exceed quality metrics, rewarding for patient outcomes that meet certain targets and/or financially penalizing providers that do not reach their quality goals. Measures from the Healthcare Effectiveness Data and Information Set (HEDIS) are often used in these contracts and includes some high-value process measures like appropriate breast cancer screening and blood pressure control in patients with diabetes.19 A PFP program implemented in Michigan reduced spending by one percent and improved performance on eleven of fourteen quality measures, including high-value services like preventive care (adolescent well care, adolescent immunization, and well-child visits at ages 3–6) and four diabetes care measures.20
However, pay-for-performance programs have been criticized for incenting providers to avoid complex and vulnerable patients in order to more easily achieve their quality targets.21 A variation that rewards rates of improvement is one strategy to ensure pay-for-performance strategies continue to serve minority populations effectively.22 Risk adjusting for a patient’s socio-economic status is another strategy to ensure providers working with underserved patient populations although the technique has been criticized for being difficult to fine tune.23
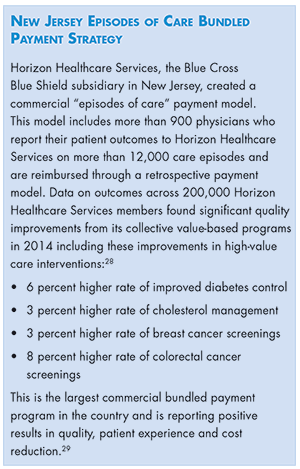
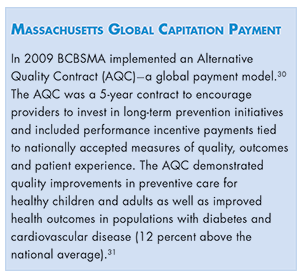
Total costs of care (also known as global payments or condition-specific capitation), is another provider reimbursement strategy that can increase use of high-value services. This approach provides a fixed price for all services needed by a specific group of people over a fixed amount of time.24 The HMO, ACO or other integrated provider organization has full accountability for the total cost and quality of care for the group of patients, creating an incentive to eliminate unneeded services and to deliver upstream care that improves outcomes.25 An example from ChenMed, a global value-based payment model, demonstrates that when providers are incentivized to provide high levels of access to preventive care, costs are lower for the practice and patient outcomes are improved.26 To reduce disparities in care and improve patient outcomes, payments under these models are often adjusted based on the health of the patient as well as other factors that may affect the level of engagement from providers, like language barriers.27 (see New Jersey and Massachusetts boxes).
Non-Financial Provider Incentives
Despite widespread emphasis on provider payment reform, provider practice patterns can also be influenced by non-financial incentives.32 For example, peer-to-peer comparisons have proven very influential in changing the practice patterns of provider outliers. Likewise, public reporting tools can hold providers and hospital systems accountable for cost and quality and introduce an element of competition where patients can shop around for providers that provide the highest value. One strategy researchers recommend to ensure that racial and ethnic biases do not affect clinical decision making is to develop evidence-based guidelines for various populations and create clinician report cards, stratified by race, ethnicity and language.33 These techniques are even more effective when financial and non-financial incentives are aligned.
Consumer Incentives
Consumers can and should be encouraged to use high-value care, consistent with their preferences and goals.
One approach is to lower out-of-pocket (cost-sharing) barriers to high-value care. The Affordable Care Act required that high-value USPSTF services with an A or B grade, like the services referenced in Table 1, be provided free of cost sharing, and early observations suggest positive health outcomes due to the increase use of these preventive services.34
Also known as value-based insurance design (VBID), this is an approach that aligns health plan cost sharing with the relative value of care. VBID was originally created as a mechanism to encourage patients with chronic conditions to adhere to their long-term treatment plans (tertiary care). For example, cost-sharing might be reduced or eliminated for high-value services like foot exams for diabetics. Conversely, VBID can mean increasing cost sharing for low-value care like an antibiotic for a viral infection.
The Healthcare Value Hub’s evidence review of VBID finds that evidence thus far is limited and mixed with respect to health outcomes but experimentation with the approach should continue.35
But non-financial nudges can be powerful too. For example, making it more convenient to get a flu shot36 or having a strong recommendation from your provider37 can measurably increase take-up of high-value services.
Community-Based Approaches
As the IOM noted, community-based prevention can be effective in ensuring that populations receive high-value care.
Accountable Communities of Health
Accountable Communities of Health (ACH) is an approach that brings together clinical and community-based organizations to achieve better population health outcomes.38 By coordinating various stakeholders and providing services outside traditional clinical settings, the model has great potential to reach a broader population and achieve better health equity.39
ACHs have flexibility to focus on specific populations and health conditions. For example, Iowa’s Community Care Coalition (C3) targeted tobacco use, alcohol abuse, diabetes and their associated social determinants of health. C3 hopes to increase the percentage of adult smokers who attempt to quit, decrease adult obesity prevalence, and increase the percent of adults with diabetes having A1c tests (several of the measures included in Table 1).40
Maine also has an Accountable Communities (AC) program as part of their larger Value-Based Purchasing strategy. Maine’s AC program contracts with providers who want to participate in this shared savings, pay-for-performance model. If the provider succeeds in reducing cost while meeting state-wide quality benchmarks, the AC shares in the savings with the provider.41 The amount of savings are tied, in part, to performance on providing preventive health services, especially for at-risk populations. Maine has reported better than average performance for all of their quality measures, compared to national data.42
There are other local initiatives that demonstrate high return on targeted investments in high-value preventative care. For example, the YMCA Diabetes Prevention Program is a cost-effective intervention designed to delay the onset of diabetes through a combination of coached lifestyle changes and medication adherence.43 Strong results from this program incentivized Medicare to begin reimbursing for this program in 2018.
Public Health Campaigns
Health campaigns can improve health literacy and increase the use of high-value care. A successful public health campaign must take physical health variables, as well as social and cultural factors, into account to successfully change behavior.44 An example of a successful public health campaign is the annual effort to encourage people to get their flu vaccines, guided by the Centers for Disease Control and Prevention (CDC) and the U.S. Advisory Committee on Immunization Practices who produce specialized materials to promote the importance of the vaccine targeted at specific populations.45
Another example of a public health campaign is the Human Papilloma Virus (HPV) vaccine campaign. HPV is responsible for around 30,000 new cancer diagnoses each year, but most cancers caused by HPV are preventable with the vaccine.46 Initial public health campaigns launched soon after the vaccine was recommended saw HPV infections in girls declined by 56 percent.47 To further extend the benefits of the vaccine, the American Cancer Society partnered with multiple National Cancer Institute- Designated Cancer Centers in 2016 on a new campaign targeting boys and girls at communities with the lowest rates of vaccinations. This campaign has the goal of vaccinating 80 percent of girls and boys aged 11 and older by 2026 (20 years after the vaccine was first released), reducing the number of HPV-related cancers by 90 percent.48
Conclusion
It is clear we need be providing more high-value care services to patients as part of our overall efforts to transform healthcare and “get utilization right.” Fortunately, our evidence base is strong with respect to the strategies that work. Borrowing from our knowledge of strategies to reduce the provision of low-value care,49 it is likely that multicomponent approaches (which align financial and non-financial incentives for both providers and patients) will be particularly successful, but this type of approach has not yet been evaluated. Another need is for increased comparative effectiveness research to reduce the vast grey areas of healthcare services which have not been classified as either low value or high value, in order to improve healthcare delivery and outcomes. But given existing evidence that high-value services are delivered too infrequently—contributing to disparities in health outcomes and in some cases leaving cost savings on the table—advocates, payers and others must demand progress.
Notes
1. Beaudin-Seiler, Beth, Lynn Quincy and Rebecca Cooper, Reducing Low-Value Care: Saving Money and Improving Health, Healthcare Value Hub (November 2018).
2. McGlynn, Elizabeth A., et al., “The Quality of Health Care Delivered to Adults in the United States,” New England Journal of Medicine (June 2003).
3. Adapted from Effective Care, A Dartmouth Atlas Project Topic Brief (2007). http://www.dartmouthatlas.org/downloads/reports/effective_care.pdf
4. Elshaug, Adam G., et al., “Levers for Addressing Medical Underuse and Overuse: Achieving High Value Health Care,” The Lancet, Vol. 390, No 10090 (July 2017).
5. Wal, Pranay, et al., “Management of Coronary Artery Disease in a Tertiary Care Hospital,” Journal of Basic Clinical Pharmacy, Vol. 4, No 2 (May 2013).
6. Workshop Series Summary, The Healthcare Imperative: Lowering Costs and Improving Outcomes, Institutes of Medicine (2010).
7. Maciosek, Michael V., et al., “Updated Priorities Among Effective Clinical Preventive Services,” Annals of Family Medicine, Vol. 15, No. 1 (Jan/Feb 2017).
8. Pignone, Michael P., Tertiary Prevention and Treatment Costs in The Healthcare Imperative: Lowering Costs and Improving Outcomes, Institutes of Medicine (2010).
9. Workshop Series Summary, The Healthcare Imperative: Lowering Costs and Improving Outcomes, Institutes of Medicine (2010).
11. Borsky, Amanda, et al., “Few Americans Receive All High-Priority, Appropriate Clinical Preventive Services,” Health Affairs (June 2018).
12. “Achieving Equity in Health,” Health Policy Brief, Health Affairs (Oct. 6, 2011).
13. Barnett, Michael L., et al., “Low-Value Medical Services in the Safety-Net Population,” JAMA Network, Vol. 166, No. 6. (June 2017).
14. Tricoci, Pierluigi, et al., “Scientific Evidence Underlying the ACC/AHA Clinical Practice Guidelines,” JAMA, Vol. 301, No. 8, (February 2009).
15. Steel, Nicholas., et al., “A Review of Clinical Practice Guidelines Found That They Were Often Based on Evidence of Uncertain Relevance to Primary Care Patients,” Journal of Clinical Epidemiology, Vol. 67, No. 11, (November 2014).
16. Beaulieu, Nancy, et al., “The Economics of Paying for Value,” Health Affairs Blog (March 2016).
17. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, Health Plan Implementation of U.S. Preventive Services Task Force A and B Recommendations (Oct. 7, 2011). https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6039a3.htm
18. “Pay-for-Performance,” Health Policy Brief, Health Affairs (Oct. 11, 2012).
19. Caveney, Brian J., “Pay-for-Performance Incentives: Holy Grail or Sippy Cup?” North Carolina Medical Journal, Vol. 77, No. 4 (August 2016).
20. Lemak, Christy, et al., “Michigan’s Fee-For-Value Physician Incentive Program Reduces Spending and Improves Quality in Primary Care,” Health Affairs. Vol. 34, No. 4. (April 2015).
21. Weissman, Joel S., et al., Healthcare Disparities and Measurements, National Quality Forum (February 2012).
22. Sura, Amit, and Nirav Shah, “Pay-for-Performance Initiatives: Modest Benefits for Improving Healthcare Quality,” American Health & Drug Benefits, Vol. 3, No. 2 (April 2010).
23. University of Minnesota, Disparities and Risk Adjustment, http://p4presearch.umn.edu/controversial-issues/disparities-and-risk-adjustment (accessed on Oct. 15, 2018).
24. Center for Healthcare Quality and Payment Reform, Which Healthcare Payment System is Best?, http://www.chqpr.org/downloads/whichpaymentsystemisbest.pdf
25. James, Brent C., and Gregory Poulsen, “The Case for Capitation,” Harvard Business Review (August 2016).
26. ChenMed, How High-Touch Care Improves Outcomes and Reduces Cost (September 2017). https://www.chenmed.com/sites/jencare/files/ChenMed%2520Report%252C%2520Concierge%2520Care%2520for%2520Low-Income%2520Seniors.pdf (accessed Nov. 6, 2018).
27. Miller, Harold D., “From Volume to Value: Better Ways to Pay for Health Care,” Health Affairs, Vol. 28, No. 5 (October 2009).
28. Health Care Incentives Improvement Institute, Case Study: Horizon Healthcare Services: Nation’s Largest Commercial Value-Based Healthcare Program Delivers on Triple Aim (2015) http://prometheusanalytics.net/sites/default/files/attachments/Horizon-Prometheus-Case-Study-4-Feb-2015.pdf
29. Martinez, Julia C., Martha King and Richard Cauchi, Improving the Health Care System: Seven State Strategies, National Conference of State Legislatures, Washington, D.C. (July 2016).
30. Song, Zirui, et al., “Health Care Spending and Quality in Year 1 of the Alternative Quality Contract,” The New England Journal of Medicine, Vol. 365. (September 2011).
31. Agency for Healthcare Research and Quality, Blue Cross Blue Shield of Massachusetts Alternative Quality Contract, https://www.ahrq.gov/workingforquality/priorities-in-action/bcbsma-alternative-quality-contract.html (accessed on Oct. 15, 2018).
32. Hunt, Amanda, Non-Financial Provider Incentives: Looking Beyond Provider Payment Reform, Research Brief No. 24, Healthcare Value Hub (February 2018).
33. Bentacourt, J.,” In Pursuit of High-Value Healthcare: The Case for Improving Quality and Achieving Equity in a Time of Healthcare Transformation,” Frontiers of Health Services Management, Vol. 30, No. 3, (Spring 2014).
34. Han, Zuesong, “Has Recommended Preventive Service Use Increased After Elimination of Cost-Sharing as Part of the Affordable Care Act in the United States?” Preventive Medicine, Vol. 78. (September 2015).
35. Healthcare Value Hub, Value Based Insurance Design: Potential Strategy for Lower Costs, Increased Quality, Easy Explainer No 5 (July 2016).
36. Holland, Roberta, “How to Nudge People into Getting Their Flu Shots,” Forbes (Oct 5, 2016).
37. Lu, Peng, “Association of Provider Recommendation and Offer and Influenza Vaccination among Adults Aged ≥18 Years—United States,” Science Direct (February 2018).
38. Jones, Shyloe, Community Level, Multi-Stakeholder Approaches to Improve Healthcare Value, Research Brief No. 26, Healthcare Value Hub (May 2018).
39. Spencer, Anna, and Bianca Freda, Advancing State Innovation Model Goals Through Accountable Communities for Health, Center for Health Care Strategies, Trenton, N.J. (October 2016). https://www.chcs.org/media/SIM-ACH-Brief_101316_final.pdf
40. Iowa Department of Human Services, Community Care Coalition Initiative (April 2016). https://dhs.iowa.gov/sites/default/files/Compiled_program_factsheets.pdf
41. MaineCare Services, Accountable Communities Initiative, https://www.maine.gov/dhhs/oms/vbp/accountable.html (accessed on Nov. 6, 2018).
42. Agency for Healthcare Research and Quality, Maine State Snapshot, https://nhqrnet.ahrq.gov/inhqrdr/Maine/snapshot/table/All_Measures/All_Topics, (accessed on Nov. 6, 2018).
43. National Institute of Diabetes, Digestive and Kidney Diseases, Diabetes Prevention Program, Bethesda, MD. https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp
44. Parvanta, Claudia E., et al., Essentials of Public Health Communications, http://samples.jbpub.com/9780763771157/71157_FMxx_00i_xxxiv.pdf (accessed on Oct. 21, 2018).
45. Centers for Disease Control and Prevention, Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP), https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5306a1.htm (accessed on Oct. 21, 2018).
46. Siteman Cancer Center, Siteman Cancer Center Among Leading Institutions Encouraging HPV Vaccination, https://siteman.wustl.edu/siteman-cancer-center-among-leading-institutions-encouraging-hpv-vaccination/ (accessed on Oct. 21, 2018).
47. Centers for Disease Control and Prevention, HPV Safety and Effectiveness, https://www.cdc.gov/vaccines/vpd/hpv/hcp/safety-effectiveness.html (Accessed on Nov 6, 2018).
48. Centers for Disease Control and Prevention, HPV Vaccination: What Everyone Should Know, https://www.cdc.gov/vaccines/vpd/hpv/public/index.html (accessed on Oct. 21, 2018) and Siteman Cancer Center, Program for the Elimination of Cancer Disparities, St. Louis, MO (June 2018). https://siteman.wustl.edu/wp-content/uploads/2018/08/PECaD-stakeholders-report-1718-final-compressed.pdf
49. Beaudin-Seiler, Beth, Lynn Quincy and Rebecca Cooper, Reducing Low-Value Care: Saving Money and Improving Health, Research Brief No, 32, Healthcare Value Hub (November 2018).