Just What the Doctor Ordered: State and Local Strategies to Advance Health Equity
Health inequities—systemic differences in the health status of different population groups—continue to plague the United States’ health system. Black, Hispanic/Latino, Native Hawaiian/Pacific Islander and Native American/Alaska Native populations experience significant health inequities in the form of higher uninsured rates, higher rates of chronic conditions, less access to care, fewer high-quality care options and poorer health outcomes.1 Health inequities are also stratified by income in the U.S., further exacerbating racial and ethnic disparities, as BIPOC (Black, Indigenous and People of Color) communities experience higher rates of poverty than white communities.2, 3
Why do Health Inequities Exist?
Structural racism has created and fostered health inequities, in large part, by influencing social determinants of health (SDoH).4, 5 Though past policies such as redlining and educational/occupational segregation are no longer explicitly legal, their legacies remain in the racial and economic segregation of neighborhoods, persistent racial disparities in income and poverty, unequal access to quality education and higher education.6, 7, 8, 9 By detrimentally shaping the environments in which people—particularly people of color—live, work, learn and play, structural racism plays a large role in diminishing health.
Structural racism in the U.S. health system exacerbates these inequities by providing care that is financially prohibitive, inaccessible, of inconsistent quality and oftentimes racist. Non-white racial and ethnic groups are more likely to receive low-value care and receive fewer effective medical services, and racial gaps in health insurance coverage persist despite gains from the Affordable Care Act (ACA).10, 11, 12 Moreover, the high cost of coverage and care causes low-income earners to delay or forgo care at higher rates than others, with non-white, non-elderly individuals more likely than whites to do so.13, 14 Additionally, implicit bias and racism shapes providers’ behavior, resulting in differences in medical treatment along racial, ethnic and other demographic lines.15
The Role of State & Local Governments
Decreasing health inequities, with the goal of eliminating them, is a moral imperative of state and local governments—with their regulatory authority over systems that perpetuate health inequities, their capacity to investigate and identify community needs and their ability to develop programs tailored to address specific health priorities—who are uniquely positioned to advance this work. This research brief highlights some promising strategies gaining traction, including:
- Implementing “Racial Equity Impact Statements” for legislation, particularly in the environmental, health and criminal justice arenas;
- Requiring “Health Impact Assessments” attached to legislation to include equity considerations;
- Declaring racism a public health crisis and implementing steps to address it;
- Adopting a “Health in All Policies” approach to government decision making;
- Establishing “Health Equity Zones” to better address SDoH;
- Employing Medicaid 1115 and/or 1915 waivers to better address SDoH; and
- Implementing participatory budgeting for initiatives that focus on health and SDoH.
An extensive list of other ways that state and local governments can advance health equity is provided in the Healthcare Value Hub’s Health Equity Policy Checklists, available at https://healthcarevaluehub.org/advocate-resources/health-equity-checklists
Racial Equity Impact Statements
Racial Equity Impact Statements can be incorporated into the state and/or local legislative process to systematically examine “how different racial and ethnic groups will likely be affected by a proposed action or decision.”16 These assessments are used to evaluate and avoid unintended, inequitable consequences of proposed policies, practices, programs, plans and budgetary decisions.17 Racial Equity Impact Statements have traditionally been used at the state level to assess the equity implications of legislation concerning criminal justice reform. For example, Connecticut’s 2018 law allows members of the state’s General Assembly to request racial and ethnic impact statements for bills and amendments that could increase or decrease the pre-trial or sentenced population of the state’s correctional facilities.18
Evidence of persistent and immense health inequities indicates that these statements should also be used to assess the impact of related proposals on historically under-resourced and marginalized populations. The Montgomery County Council in Maryland pioneered this approach when it passed a bill in 2019 requiring an equity impact statement detailing a proposal’s impact on equity across different demographic groups to be produced for all new bills and budget measures.19 The City of Long Beach, California has also announced a goal of including equity impact assessments in all city staff reports prior to making policy changes. The assessments must describe the racial and economic impacts of the proposed policy change on various groups, identify how members of those groups have been engaged and include disaggregated data or information to help staff identify which groups will be most affected.20
Requiring Racial Equity Impact Statements for a broader swatch of legislation, beyond criminal justice reform, would allow state and local policymakers to better understand whether proposals will have a disparate impact on residents’ health and well-being. Though examples of this strategy currently exist only at the local level, there is momentum for implementation at the state level. In New Mexico, legislation was introduced in 2021 that would require the state’s Cultural Affairs Department to provide social, racial and cultural impact statements to the legislature for all pending legislation.21, 22
Equity-Focused Health Impact Assessments
Health Impact Assessments (HIAs) are a mechanism for policymakers to analyze proposed policies, plans or programs before implementation to determine future health implications.23 HIAs can also help policymakers better understand the disparate health impacts that a policy, plan or program may have on different racial and/or ethnic groups within a community. Equity-focused HIAs that consider existing inequities and community histories are valuable because they help avoid exacerbating existing disparities and perpetuating harm. By focusing on equity within HIAs, states can better serve historically marginalized communities, whose specific experiences and needs have for too long been overlooked and, therefore, warrant particular consideration.
While equity-focused HIAs and racial equity impact statements may appear similar in concept, they are different in their application. For example, HIAs can be used to bridge policy areas by incorporating health considerations into decision making within sectors traditionally viewed as unrelated to health, such as transportation and housing, as a means to address social determinants of health. Equity-focused HIAs go a step further, in recognition that some members of a community may be disproportionately harmed by policy or action.
|
Strategy in Action: In 2014, the City Council in Denver, Colorado decided to prioritize HIAs in forthcoming budgets for all new neighborhood plans.24, 25 Many of these HIAs provided neighborhood-level data on health disparities and considered the impacts of proposed projects on health equity. The Harris County Built Environment Unit in Harris County, Texas regularly conducts HIAs to evaluate how changes in city ordinances and community design could unequally impact the health of different community groups.26 |
Declaring Racism a Public Health Crisis
The historic oppression of Black, Indigenous, Hispanic, Latino, Asian, Pacific Islander and other non-white groups profoundly affects the health of individuals in these communities. Racist policies have impacted, and continue to impact, SDoH such as housing, food security, economic security, the environment and more. In addition, exposure to persistent racial discrimination has been shown to negatively impact health outcomes.27
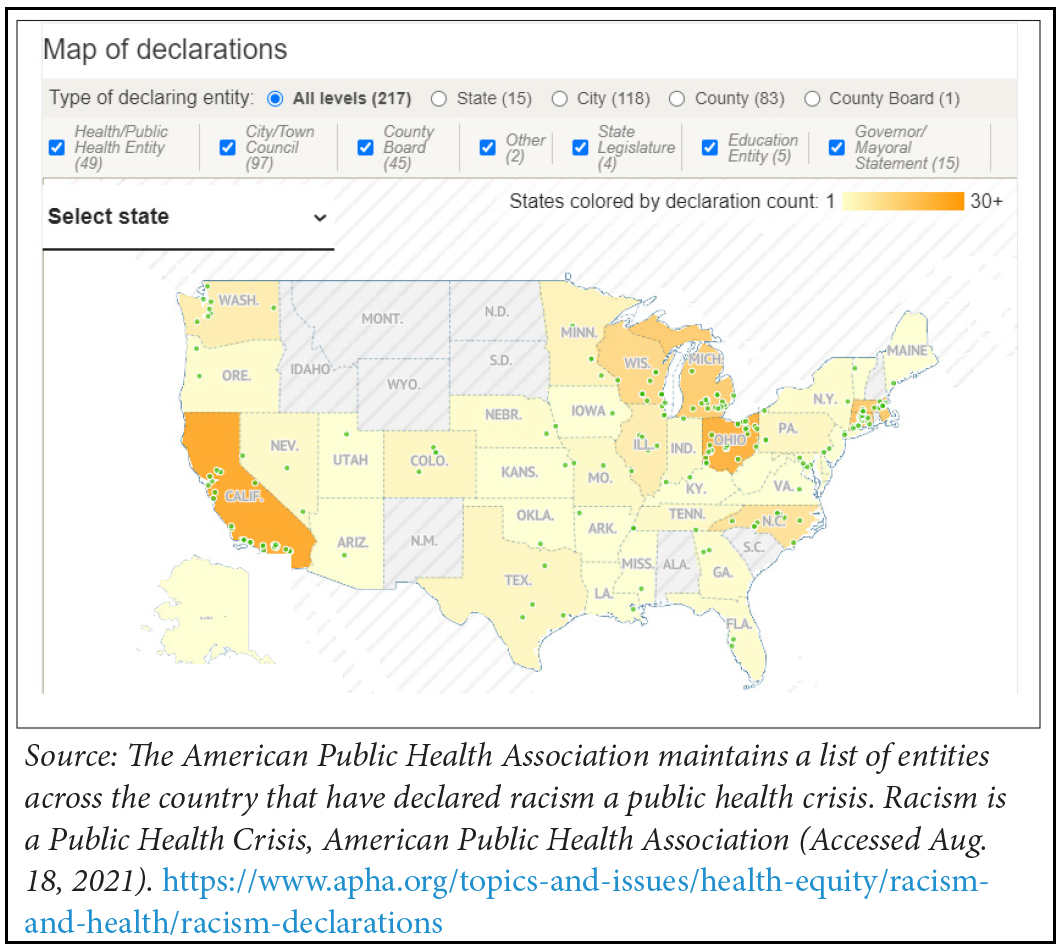
Recent events—such as the Black Lives Matter movement in response to police brutality against Black individuals and the disparate influence of COVID-19 on BIPOC communities—have highlighted the devastating effects of both overt and covert racism on the health of BIPOC individuals. In response, a growing number of local and state governments have issued statements declaring racism a public health crisis, with pledges to fight racism’s impacts on the health of underserved communities by improving health equity and reducing health disparities through concrete plans of action.
Declarations of racism as a public health crisis are only as meaningful as subsequent steps to undo existing racist policies and prevent their passage in the future. HUBCurrently, local and state governments’ plans of action vary significantly, warranting future evaluation to determine evidence-based practices. For example, Cook County, Illinois’ Board of Commissioners convened a Racial Equity Leadership Council to advance equity work within the administration after declaring racism a public health crisis.28 DeKalb County, Georgia issued a similar declaration, with a renewed commitment to focus on racial equity in policymaking. Specific goals, objectives and an equity study are forthcoming.29 At the state level, the governors of Michigan and Nevada have issued executive directives/proclamations declaring racism a public health crisis and requiring immediate action.30 Michigan’s governor issued an executive directive creating the Black Leadership Advisory Council to advise the governor and develop, review and recommend policies and actions to dismantle and prevent discrimination and racial inequity within the state.31 The Nevada governor’s proclamation mirrored the state legislature’s resolution, which requests that federal funding be distributed equitably in direct proportion to disadvantages by individual racial category. It also requests that the legislature incorporate systemic racism and the structures of racial discrimination into the business of the next regular session.32
Health in All Policies
The American Public Health Association defines Health in All Policies as “a collaborative approach to improving the health of all people by incorporating health considerations into decision-making across sectors and policy areas.”33 The goal is to encourage policymakers and other decisionmakers to think about the health, equity and sustainability impacts of different policy options across a variety of sectors. Health in All Policies strategies can take two forms: the first resembling cross-sector collaboration on a project, policy, program or response, and the second being a comprehensive approach to changing government structures and processes to routinely consider health.34 As such, Heath in All Policies initiatives can take many forms, and can be adopted both within and across agencies at the local or state level.
Health in All Policies initiatives have been gaining steam over the past few years. In 2012, the Boston Public Health Commission convened a Health in All Policies Task Force, which sought to incorporate health considerations into decision-making across all of the agencies and organizations that influence community design (for example, transportation and development), and engage residents in the process.35 A year before, Baltimore City’s Health Department created the Cross-Agency Health Taskforce to encourage agencies to promote health through a variety of policies, program designs, standard operating procedures and internal practices.36 In 2014, Ingaham County, Michigan’s Board of Health passed a resolution encouraging the Board of Commissioners to incorporate a Health in All Policies approach into their decision-making process.37, 38
State-level examples include California’s Health in All Policies Task Force—established through executive order in 2010—that brought together representatives from major state agencies to identify priorities for improving the health of Californians and produce a report outlining program and policy recommendations.39 The task force is located within the Strategic Growth Council and has facilitated several cross-agency, statewide initiatives focused on healthy food, transportation and creating violence-free and resilient communities, among other topics.40
Health Equity Zones
Rhode Island’s innovative Health Equity Zone (HEZ) initiative uses a community-led process to conduct needs assessments and implement data-driven action plans to address social, economic and environmental factors impacting health in high-need communities.41 Nine HEZ collaboratives located throughout the state each bring together a diverse group of community stakeholders to identify the health-related needs of their communities and develop and promote programs, services and initiatives to address those needs.42 Bristol’s HEZ, for example, created programs focused on food and nutrition; physical activity; substance abuse awareness and prevention; and personal health and wellness in response to community need.43 Additionally, the HEZ facilitated the passage and implementation of a town-wide ordinance banning cigarettes and vaping in all town parks, ensuring access to smoke-free public spaces. Bristol’s HEZ also runs a drop-in recovery center, offering trainings, support groups and social events for those struggling with substance use or recovery.
Maryland implemented a similar Health Enterprise Zone initiative through the Maryland Health Improvement and Disparities Reduction Act of 2012, which successfully operated through 2016. The initiative was associated with a significant reduction in inpatient hospital stays and a net savings of $93.4 million for Maryland’s healthcare system.44 While an increase in emergency department visits was also observed, researchers posit that this resulted from: (1) patients who had previously not sought healthcare beginning to do so due to the awareness the HEZ raised in the community and (2) patients who normally would have been admitted to the hospital through the emergency department (thereby being given inpatient status) being sent home due to newly available follow-up resources in the community. Both residents and providers reported positive experiences—including improved health outcomes associated with diabetes, cardiovascular-related illness and other chronic conditions—resulting from a variety of community-based solutions. Despite the program’s success, funding was not renewed after 2016.
In 2021, Maryland passed the Health Equity Resource Act to create and fund Health Equity Resource Communities to reduce racial disparities in health outcomes by improving access to care, building upon the previous success of the Health Enterprise Zone initiative.45, 46 The Act also establishes the Pathways to Health Equity program, which will provide a foundation and guidance for a permanent Health Equity Resource Community program and provide grants to: reduce health disparities; improve health outcomes and access to primary care; promote preventive services; and reduce healthcare costs and hospital admissions/readmissions.47 States looking to follow Rhode Island and Maryland’s example should first investigate specific health disparities that exist among different communities, as well as community capacity and assets.
Address Social Determinants of Health with Medicaid 1115 and/or 1915 Waivers
Medicaid demonstration waivers provide an excellent opportunity for states to promote health equity by addressing social determinants of health (SDoH). Section 1115 Medicaid demonstration waivers grant states the flexibility to test new healthcare delivery approaches—under section 1115 research and demonstration authority, the Secretary of the U.S. Department of Health and Human Services may waive certain provisions of Medicaid and Children’s Health Insurance Program statutes related to state program design.48 While some states use section 1115 waivers to fund the provision of health-related social services (like non-emergency medical transportation) to individuals with Medicaid coverage, other states use 1115 waivers to implement payment and delivery reforms that seek to incentivize plans and providers to address SDoH. Section 1915 waivers targeting people who need long-term services and supports can also be used to address SDoH, particularly 1915(c) waivers authorizing states to provide home and community-based services as an alternative to institutional care in nursing homes, hospitals and intermediate care facilities for individuals with intellectual disabilities.49
|
Strategy in Action Prior to the program ending in 2020, New York used the Delivery System Reform Incentive Payment (DSRIP)50 program authorized under Section 1115 authority to integrate clinical providers with behavioral health, community and social support organizations across the state. DSRIP funding for the 25 regional Performing Provider Systems (PPS) allowed coordinating organizations to receive payment for services that otherwise would not have garnered Medicaid funding, allowing community-based organizations like food banks, homeless shelters and community health centers to work in concert with providers to help address patients' needs.51, 52 North Carolina's Section 1115 waiver funds Healthy Opportunities Pilots, covering evidence-based non-medical services addressing specific health-related social needs, like housing, transportation, food insecurity, interpersonal violence and toxic stress.53 Wisconsin implemented a 1915(c) Self-Directed Support Waiver to provide housing counseling, housing start-up and utility costs, including relocation, to people with developmental or intellectual disabilities, older adults and disabled individuals.54 |
While Medicaid waivers like those highlighted in the box to the right can be used to promote health equity and address SDoH, they have also been used to implement Medicaid work requirements, which undermine health equity goals. A study of Arkansas’ Medicaid work requirements revealed that 50 percent of state residents aged 30-49 who had lost Medicaid coverage in the prior year due to work requirements reported serious problems paying off medical debt. Fifty-six percent delayed care due to cost and 64 percent delayed taking medications due to cost.55 Furthermore, the well-documented administrative errors that have resulted in eligible recipients losing their Medicaid coverage has particularly devastating consequences for individuals with disabilities, who often rely on access to regular care to manage their conditions.56 States can better serve their residents by using Medicaid 1115 and 1915 waivers to address SDoH and improve health equity, for example, by increasing the provision of health-related supports.
Participatory Budgeting
Participatory budgeting “is a democratic process in which community members decide how to spend part of a public budget.”57 Participatory budgeting can increase equity by directly involving residents who have traditionally been underserved, ignored or harmed by policies and giving them the resources they need to improve their communities. Drawing from their lived experiences, community members are best equipped to bring innovative and relevant solutions to the forefront of budgeting discussions. Because many participatory budgeting initiatives do not restrict resident voting eligibility as stringently as political elections, often-ignored groups, such as people without documentation, formerly incarcerated individuals and youth can contribute their unique perspectives, increasing the diversity of voices who have a say in how funds are spent. This collaborative and community-driven process helps ensure that community members’ needs are heard and addressed.58
In Brazil, participatory budgeting has been associated with “a reduction in extreme poverty, better access to public services, greater spending on sanitation and health services and a reduction in child and infant mortality.”59 While participatory budgeting is a relatively new concept in the U.S., numerous communities around the country are embracing the process to better address community needs, including those related to health. The Tacoma-Pierce County Health Department in Washington60 has initiated participatory budgeting projects in three schools in Eastside Tacoma, one of the county’s highest-need communities.61 The city government is also piloting a participatory budgeting project in Eastside Tacoma, allowing the community to decide how to spend $100,000 for neighborhood improvement projects. In Louisville, Kentucky, residents of Districts 6 and 8 involved in a participatory budgeting initiative prioritized sidewalk repairs.62 Participatory budgeting in St. Louis, Missouri has funded community projects related to violence prevention, youth engagement, mental health, peer support and trauma-informed care. In addition, the City of Vallejo, California has allocated more than $8.3 million to participatory budgeting projects since 2012, funding parks and recreation improvements, street and city cleanup, community gardens and nutrition education, the Omega Boys & Girls Club Gym renovation, school meal improvements, after school sports programs and more.63
To emphasize equity, participatory budgeting initiatives should seek to maximize community involvement, particularly for historically marginalized groups that suffer from health inequities, such as BIPOC individuals and immigrant communities. Community members should be involved in all stages of the process, including issue discussion, decision-making, implementation and evaluation.64, 65
Conclusion
Health disparities continue to harm BIPOC communities across the country and will continue to do so until state and local governments take bold action. While the influx of policies aiming to improve health equity over the past several years is encouraging, future study is needed to identify “gold standard” strategies as well as best practices for each particular approach. Still, common-sense practices—such as considering how proposed policies may disproportionately impact community residents; addressing the breadth of factors that contribute to health; and increasing community involvement in health policy decisions—will likely make meaningful strides towards improving health equity. To see how well your state’s policy environment supports health equity and to identify areas for improvement, please view the Healthcare Value Hub’s Health Equity Policy Checklists at https://healthcarevaluehub.org/advocate-resources/health-equity-checklists.
Notes
1.Carratala, Sofia, Health Disparities by Race and Ethnicity, Center for American Progress (May 7, 2020). https://www.americanprogress.org/issues/race/reports/2020/05/07/484742/health-disparities-race-ethnicity/
2. Schneider, Eric C., et al., Mirror Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care, The Commonwealth Fund (July 2017) https://interactives.commonwealthfund.org/2017/july/mirror-mirror/
3. State Health Facts: Poverty Rate by Race/Ethnicity: 2019, Kaiser Family Foundation (Accessed June 8, 2021). https://www.kff.org/other/state-indicator/poverty-rate-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
4. Bailey, Zinzi D., et al., “Structural Racism and Health Inequities in the USA: Evidence and Interventions,” The Lancet (April 8, 2017). https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)30569-X/fulltext
5. Artiga, Samantha, and Elizabeth Hinton, Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity, Kaiser Family Foundation (May 10, 2018). https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/
6. Mitchell, Bruce, and Juan Franco, HOLC “Redlining” Maps: The Persistent Structure of Segregation and Economic Inequality, NCRC (March 20, 2018). https://ncrc.org/wp-content/uploads/dlm_uploads/2018/02/NCRC-Research-HOLC-10.pdf
7. Wilson, Valerie, Racial Disparities in Income and Poverty Remain Largely Unchanged Amid Strong Income Growth in 2019, Economic Policy Institute Working Economics Blog (Sept. 16, 2020). https://www.epi.org/blog/racial-disparities-in-income-and-poverty-remain-largely-unchanged-amid-strong-income-growth-in-2019/
8. Darling-Hammond, Linda, Unequal Opportunity: Race and Education, Brookings Institute (March 1, 1998). https://www.brookings.edu/articles/unequal-opportunity-race-and-education/
9. Weller, Christian E., African Americans Face Systematic Obstacles to Getting Good Jobs, Center for American Progress (Dec. 5, 2019). https://www.americanprogress.org/issues/economy/reports/2019/12/05/478150/african-americans-face-systematic-obstacles-getting-good-jobs/
10. Schpero, William L., et al., “For Selected Services, Blacks and Hispanics More Likely to Receive Low-Value Care Than Whites,” Health Affairs, Vol. 36, No. 6 (June 2017). https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2016.1416
11. Andrews, Michelle, “Quantity Over Quality? Minorities Shown to Get an Excess of Ineffective Care,” Kaiser Health News (June 9, 2017). https://khn.org/news/quantity-over-quality-minorities-shown-to-get-an-excess-of-ineffective-care/
12. Artiga, Samantha, et al., Health Coverage by Race and Ethnicity, 2010-2019, Kaiser Family Foundation (July 16, 2021). https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/
13. Ndugga, Nambi, and Samantha Artiga, Disparities in Health and Health Care: 5 Key Questions and Answers, Kaiser Family Foundation (May 11, 2021). https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question-and-answers/
14. See: Tennessee Residents Struggle to Afford High Healthcare Costs; COVID Fears Add to Support for a Range of Government Solutions Across Party Lines, Data Brief No. 94, Healthcare Value Hub (July 2021) https://healthcarevaluehub.org/tennessee-state-survey; and Oregon Residents Struggle to Afford High Healthcare Costs; COVID Fears Add to Support for a Range of Government Solutions Across Party Lines, Data Brief No. 91, Healthcare Value Hub (June 2021) https://healthcarevaluehub.org/oregon-state-survey; and Pennsylvania Residents Struggle to Afford High Healthcare Costs; COVID Fears Add to Support for a Range of Government Solutions Across Party Lines, Data Brief No. 89, Healthcare Value Hub (February 2021) https://healthcarevaluehub.org/pennsylvania-state-survey
15. Chapman, Elizabeth N., et al., “Physicians and Implicit Bias: How Doctors May Unwittingly Perpetuate Health Care Disparities,” Journal of General Internal Medicine, Vol. 28, No. 11 (November 2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3797360/
16. Racial Equity Impact Assessment, Race Forward, (2009). https://www.raceforward.org/sites/default/files/RacialJusticeImpactAssessment_v5.pdf
17. Ibid.
18. Public Act No. 18-78: An Act Concerning Racial and Ethnic Impact Statements, Connecticut Senate Bill No. 256 (June 1, 2018). https://www.cga.ct.gov/2018/ACT/pa/2018PA-00078-R00SB-00256-PA.htm
19. Agenda Item #5A: Bill 27-19, Montgomery County Council (Nov. 19, 2019). https://www.montgomerycountymd.gov/council/Resources/Files/agenda/col/2019/20191119/20191119_5A.pdf
20. Racial Equity and Reconciliation Initiative: Initial Report, City of Long Beach (Aug. 3, 2020). https://www.longbeach.gov/globalassets/health/media-library/documents/healthy-living/office-of-equity/reconciliation/report-racial-equity-and-reconciliation-intiative
21. Senate Bill 55, New Mexico 2021 Regular Session (Accessed June 8, 2021). https://www.nmlegis.gov/Legislation/legislation?chamber=S&legType=B&legNo=55&year=21
22. As of publication, this bill was reported by the Senate Indian, Rural and Cultural Affairs Committee with a ”do pass” recommendation and referred to the Senate Finance Committee. See above citation.
23. Heller, Jonathan, et al., Promoting Equity through the Practice of Health Impact Assessment, PolicyLink (2013). https://hiasociety.org/resources/Documents/HIA-Promoting-Equity.pdf
24. Denver Department of Public Health & Environment, Health Impact Assessment (Accessed June 8, 2021). https://www.denvergov.org/content/denvergov/en/environmental-health/our-divisions/community-and-behavioral-health/health-impact-assessment.html#:~:text=A%20health%20impact%20assessment%20(HIA,is%20adopted%2C%20built%20or%20implemented.&text=HIAs%20are%20being%20used%20to,through%20community%20design%20and%20development
25. Armijo, Gretchen, and Maggie Kauffman, “Health in All Policies in Denver, CO: Moving from Plans to Equitable Development Outcomes,” Chronicles of Health Impact Assessment, Vol. 4, No 1 (October 2019). http://journals.iupui.edu/index.php/chia/article/view/23703/22861
26. Harris County Public Health, HIA Case Studies (Accessed June 8, 2021). https://publichealth.harriscountytx.gov/Resources/Built-Environment-Toolkit/Health-Impact-Assessment/HIA-Case-Studies
27. David R. Williams, Why Discrimination is a Health Issue, Robert Wood Johnson Foundation (May 26, 2021). https://www.rwjf.org/en/blog/2017/10/discrimination-is-a-health-issue.html
28. Cook County Government, Health & Hospitals Committee Meeting July 24, 2019 (Accessed June 8, 2021). https://cook-county.legistar.com/MeetingDetail.aspx?ID=711467&GUID=1BEC6AE5-4212-430F-B5A3-AD36CB6FAA41&Options=&Search=
29. Tyler Estep, “DeKalb County Declares Racism a Public Health Crisis,” Atlanta Journal-Constitution (July 22, 2020). https://www.ajc.com/news/atlanta-news/dekalb-county-declares-racism-a-public-health-crisis/QPDAOVI36VCW3D4XD4MXVN3WOM/
30. State Legislation to Declare Racism a Public Health Crisis and Address Institutional Racism, Association of State and Territorial Health Officials (Aug. 12, 2020). https://www.astho.org/StatePublicHealth/State-Legislation-to-Declare-Racism-a-Public-Health-Crisis-and-Address-Institutional-Racism/08-12-20/
31. Governor Whitmer Signs Executive Directive Recognizing and Addressing Racism as a Public Health Crisis, Creates the Black Leadership Advisory Council, Office of Governor Gretchen Whitmer (Aug. 5, 2020). https://www.michigan.gov/whitmer/0,9309,7-387-90499-535762--,00.html
32. Nguyen, Khanh, “Nevada Declares Racism a Public Health Crisis, Other States Explore Similar Action,” State Legislatures Magazine (Sept. 28, 2020). https://www.ncsl.org/bookstore/state-legislatures-magazine/nevada-declares-racism-a-public-health-crisis-other-states-explore-similar-action-magazine2020.aspx
33. Health in All Policies: A Guide for State and Local Governments, American Public Health Association (Accessed Aug. 20, 2021). https://www.apha.org/-/media/Files/PDF/factsheets/Health_inAll_Policies_Guide_169pages.ashx
34. Health in All Policies: A Framework for State Health Leadership, Association of State and Territorial Health Officials (Accessed June 8, 2021). https://www.astho.org/HiAP/Framework/
35. Boston Public Health Commission, Health in All Policies (Accessed June 8, 2021). http://www.bphc.org/whatwedo/healthy-eating-active-living/health-in-all-policies/Pages/default.aspx
36. Baltimore City Health Department, Cross Agency Health Taskforce (CAHT) (Accessed June 8, 2021). https://health.baltimorecity.gov/node/1451
37. Health in All Policies: A Framework for State Health Leadership, Association of State and Territorial Health Officials (Accessed June 8, 2021). https://www.astho.org/HiAP/Framework/
38. Ingaham County Board of Health, Resolution in Support of Adopting a Health-in-All-Policies Approach to Decision-Making in Ingham County Government (Accessed June 8, 2021). https://hd.ingham.org/Portals/HD/Home/Documents/boh/Resolutions/HIAP%20Reso.pdf
39. Incorporating Health into Policymaking Across Sectors: The California Health in All Policies Initiative, Center for Health Care Strategies (May 2018). https://www.chcs.org/resource/incorporating-health-into-policymaking-across-sectors-the-california-health-in-all-policies-initiative/
41. Health Equity Zones, Rhode Island Department of Health (August 2018). https://health.ri.gov/publications/brochures/HealthEquityZones.pdf
42. Health Equity Zones: A Toolkit for Building Healthy and Resilient Communities, Rhode Island Department of Health (Accessed Aug. 18, 2021). https://health.ri.gov/publications/toolkits/health-equity-zones.pdf
43. Bristol Health Equity Zone (HEZ), Rhode Island Department of Health (Accessed Aug. 18, 2021). https://health.ri.gov/programs/detail.php?pgm_id=1109
44. Bullard, Alyssa Jasmine, et al., Achieving Health Equity: Health Impact of Maryland’s Health Enterprise Zones: White Paper, Johns Hopkins Center for Health Disparities Solutions (Sept. 10, 2020). https://healthcareforall.com/wp-content/uploads/2020/09/HEZ-White-Paper_2020.09.10_Final-1.pdf
45. SB 172, The Maryland Health Equity Resource Act, 2021 Regular Session (2021). https://mgaleg.maryland.gov/mgawebsite/Legislation/Details/SB0172?ys=2021RS
46. Maryland Citizen’s Health Initiative, Health Equity Resource Communities (Accessed April 27, 2021). https://healthcareforall.com/get-involved/equitycommunities/
47. SB 172, The Maryland Health Equity Resource Act, 2021 Regular Session (2021). https://mgaleg.maryland.gov/mgawebsite/Legislation/Details/SB0172?ys=2021RS
48. Waivers, Medicaid and CHIP Payment and Access Commission (MACPAC) (Accessed June 9, 2021). https://www.macpac.gov/medicaid-101/waivers/
49. Ibid.
50. The DSRIP program ended on March 31, 2020.
51. Daniel-Robinson, Lekisha, and Jennifer E. Moore, Innovation and Opportunities to Address Social Determinants of Health in Medicaid Managed Care, Institute for Medicaid Innovation (January 2019). https://www.medicaidinnovation.org/_images/content/2019-IMI-Social_Determinants_of_Health_in_Medicaid-Report.pdf
52. Weller, Wendy, et al., Statewide Annual Report by the Independent Evaluator for the New York State Delivery System Reform Incentive Payment (DSRIP) Program, University at Albany, State University of New York (2019). https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/annual_report_2019.pdf
53. Guth, Madeline, et al., The Landscape of Medicaid Demonstration Waivers Ahead of the 2020 Election, Kaiser Family Foundation (Oct. 30, 2020). https://www.kff.org/medicaid/issue-brief/the-landscape-of-medicaid-demonstration-waivers-ahead-of-the-2020-election/
54. State Housing and Services Options in 1915(c) Waivers for People with Developmental Disabilities, National Academy for State Health Policy (2018). https://www.nashp.org/wp-content/uploads/2018/11/Housing-and-service-options-1_24_2019.pdf
55. Sommers, Benjamin, et al., “Medicaid Work Requirements in Arkansas: Two-Year Impacts on Coverage, Employment, and Affordability of Care,” Health Affairs, Vol. 39, No. 9 (September 2020). https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2020.00538?journalCode=hlthaff
56. Wagner, Jennifer, and Jessica Schubel, States’ Experiences Confirm Harmful Effects of Medicaid Work Requirements, Center on Budget and Policy Priorities (Nov. 18, 2020). https://www.cbpp.org/research/health/states-experiences-confirm-harmful-effects-of-medicaid-work-requirements
57. What is PB?, The Participatory Budgeting Project (Accessed June 10, 2021). https://www.participatorybudgeting.org/what-is-pb/
58. PB Can: Deepen Equity and Inclusion, The Participatory Budgeting Project (Accessed June 10, 2021). https://www.pbcan.org/issues/equity-inclusion/
59. Hagelskamp, Carolin, et al., “Participatory Budgeting: Could It Diminish Health Disparities in the United States?” Journal of Urban Health, Vol. 95, No. 5 (October 2018). https://pubmed.ncbi.nlm.nih.gov/29736813/
60. Adopting Participatory Budgeting in Pierce County, Washington, PHNCI, NOTC at the University of Chicago, (April 2019). https://phnci.org/uploads/resource-files/PHNCI-Case-Study-Tacoma-Pierce-County.pdf
61. Needles, Allison, “How Should the City Spend $100k on Tacoma’s Eastside? You Decide,” The News Tribune (Feb. 26, 2020). https://www.thenewstribune.com/news/local/article240634037.html
62. Resiliency in Communities After Stress and Trauma, St. Louis ReCAST (2019). https://slaco-mo.org/wp-content/uploads/2019/04/ReCast.pdf
63. City of Vallejo, Participatory Budgeting (Accessed June 10, 2021) https://www.cityofvallejo.net/city_hall/departments___divisions/city_of_vallejo_speaker_s_bureau___bios/participatory_budgeting
64. Frances, Francisco, and Daniel La Parra-Casado, Participation as a Driver of Health Equity, World Health Organization: Europe (2019). https://apps.who.int/iris/bitstream/handle/10665/324909/9789289054126-eng.pdf?sequence=1&isAllowed=y
65. Hagelskamp, Carolin, et al., “Participatory Budgeting: Could It Diminish Health Disparities in the United States?” Journal of Urban Health, Vol. 95, No. 5 (October 2018). https://pubmed.ncbi.nlm.nih.gov/29736813/







