State News
Tennessee
Tennessee’s Health System Ranking is among the worst in the country, based on high uninsurance rates, high costs relative to household income and not getting needed care because of cost. Further, many measures of healthcare cost and quality from 2019 worsened for Tennessee compared to 2020, including avoidable hospital use and costs.
The state’s Health Care Innovation Initiative was launched in February of 2014 to promote payment reform to move from fee-for-service and towards paying for value. This work led to Tennessee’s State Innovation Model (SIM) grant—awarded in December of 2014—which focuses on engaging the majority of primary care providers in a multi-payers patient-centered medical home program. Additionally, Knoxville Area Transit was awarded $200,000 as part of the Rides to Wellness Demonstration to expand its call center as a single point of entry for older adults and people with disabilities to access transit to healthcare facilities in the region, according to the Federal Transit Administration.
The Tennessee Department of Health makes limited health related data available to the public including the Behavioral Risk Factor Survey and the Vital Statistics.
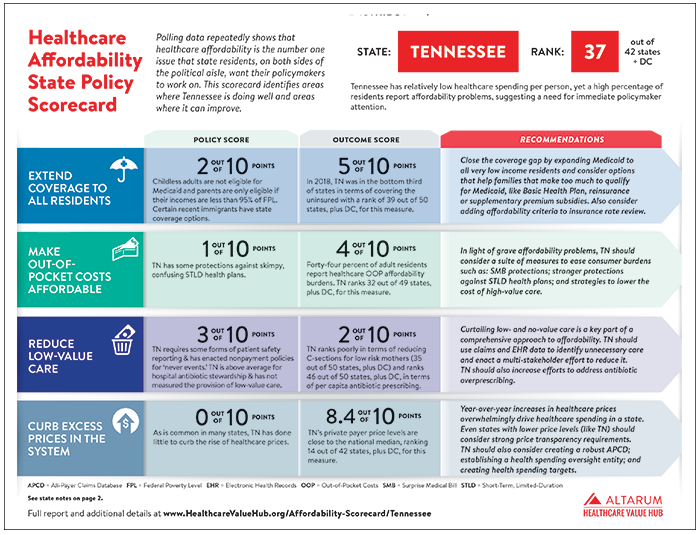
Tennessee ranked 36 out of 47 states plus DC, with a score o26.2 out of 80 possible points in the Hub's 2021 Healthcare Affordability State Policy Scorecard.
Knoxville’s Black Community Endured Deeply Rooted Racism – Now There is Medical Debt
People of color shoulder most of the medical debt throughout Knoxville, Tennessee, explains Kaiser Health News. Systemic racism and a history of segregation in areas such as East Knoxville have manifested in significantly worse health outcomes and higher rates of medical debt in communities of color; for example, more than 30 percent of the residents in the communities surveyed have a medical bill on their credit record, compared to fewer than 10 percent in white suburbs. Many of the gains in health insurance coverage due to the Affordable Care Act have remained out of reach in Knoxville.
Certificate of Need Reform Passes Tennessee General Assembly
The Tennessee General Assembly passed a certificate of need reform bill to reduce requirements and costs associated with opening, reopening or expanding a hospital, reports the Murfreesboro Post. The law changes the fee schedule associated with obtaining approval for a new healthcare service or facility, reduces the application process from 135 days to 60 days, exempts services in counties with populations above 175,000 people and allows rural hospitals to reopen without restarting the certificate of need application process.
Advocates Sue to Stop Tennessee Medicaid Block Grant Program
A group of Tennessee Medicaid recipients has filed a lawsuit seeking to halt a plan that would make contentious changes to the state's program designed to provide medical coverage to low-income earners in the state, according to Modern Healthcare. The Tennessee Justice Center — who is representing the recipients — claims the federal government exceeded its authority in approving the proposal. Block grant supporters argue that the current system gives states little incentive to control expenses because no state pays more than half the total cost. However, opponents and health advocates have expressed concern that spending caps might cause states to purge their rolls or reduce services.
Report Assesses Rural Hospital Closures in Tennessee
The Tennessee Health Care Campaign’s Rural Equity Report shows three-fourths of the state’s 25 remaining essential access rural hospitals are at high risk of closure in the next few years, reports The Rogersville Review. The report includes a toolkit for rural communities with vulnerable hospitals that offers solutions to rural health inequities, including: prioritizing infrastructure improvements in roads, broadband and emergency call centers; state oversight of hospital ownership transfers; increased financial investment in rural health; and increasing coverage for Tennesseans in rural areas. The report also includes interviews with stakeholders that share their experiences and perceptions of rural hospital closures.
CMS Approves First Medicaid Block Grant Waiver in Tennessee
Tennessee is set to become the first state to implement a Medicaid block-grant program after the Centers for Medicare and Medicaid Services (CMS) approved the state's waiver last week, according to Healthcare Finance. The block grant, called an “aggregate cap,” will create a fixed spending target based on historical enrollment and Medicaid cost data that increases at a “reasonable growth rate” over time. It will also give the state the option to exclude certain pharmaceutical drugs from the formulary. Numerous advocacy organizations, payers and providers oppose Medicaid block grants because they fear that underserved populations will lose access to healthcare by putting a cap on federal funds.
'Deep Dive' Needed Before Drawing Conclusions on Potential State Health Plan Overpayments, Tennessee Official Says
Tennessee state officials said that while a private data firm's initial findings that state health plans erroneously paid $17.58 million in medical bill overcharges were "helpful," a planned "deep dive" is necessary before drawing firm conclusions, according to Chattanooga Times Free Press. In its preliminary report in June, Connecticut-based ClaimInformatics says it found state health plans' third-party administrators BlueCross BlueShield of Tennessee and Cigna overpaid at least $17.58 million over a three-year period in bill claims by professional providers such as physicians.
Practice Agreement Requirements Temporarily Suspended and Waived
Tennessee was one of 21 states to temporarily suspend scope-of-practice requirements in an effort to expand access to care during the coronavirus pandemic, according to the American Association of Nurse Practitioners. The order, which lapsed on May 18, cleared the way for nurse practitioners to write prescriptions without consulting a physician, waived a requirement for chart review and waived a requirement that a supervising physician visit remote sites every 30 days, among other things. Nursing groups have pushed the governor to extend the executive order.
Tennessee's Secret Plentiful Coronavirus Testing? Picking Up the Tab
In Tennessee, anyone who wants a test can get one, and the state will pick up the tab. The guidance has evolved to “when in doubt, get a test,” and the state started paying for it in April, according to Kaiser Health News. Tennessee is doing more than double the minimum number of tests needed to control its outbreak, an NPR analysis states. Rather than private labs billing various health insurance plans, the state is picking up the tab at $100 per test.
A Deep Dive into Health Insurance Coverage in Tennessee
90 percent of Tennesseans had health insurance in 2018, with just over half the population getting job-based coverage through an employer, according to a report from the Sycamore Institute. Authors also noted that marketplace plans are a relatively small source of coverage in Tennessee—3 percent in 2018. Men, people of color, younger adults, the unemployed, and those with less education and income were more likely to be uninsured.
Tennessee Legislators Target Unpopular Regulation as They Look to Lower Healthcare Costs, Increase Access
A certificate of need (CON) is a permit that healthcare organizations in Tennessee must obtain from the state before building, operating or offering one of 26 regulated facilities, technologies and services. Legislators are discussing whether small tweaks or a sweeping overhaul could help or harm a fragile health care system in which 12 rural hospitals have closed since 2013, according to Chattanooga Times Free Press. Proponents of the programs argue they're needed to ensure orderly growth and limit health care spending, because health care is unlike other goods and services. However, opponents believe removing the cumbersome regulation will free the healthcare industry, bringing more providers into the market to drive competition and lower costs. A legislator working group has relied on data, stakeholder input, expert testimonies and their past experience wrestling with the law as they weigh options for changes.
New Rural Research Center Will Focus on Breaking Cycle of Poor Health
A new rural health research center in Tennessee will focus on breaking the cycle of inter-generational behavior that contributes to poor health. The Center for Rural Health Research will be housed at the College of Public Health at East Tennessee State University in Johnson City, TN, according to Daily Yonder. The center will also work to become a source for policymakers – providing the data from which those in government and other policy making organizations can make decisions to help improve the health of those in rural and nonurban communities.
Rising Hospital Costs and Shrinking Payments are Threatening Tennessee’s Hospitals
The expense of providing Tennessee residents with care is increasingly outweighing the revenue coming in, according to The Tennessean. Hospitals use gross charges—the money they charge for services before applying discounts for insurance contracts and Medicare payments, among others—as an indicator of the revenue they need to function. Gross charges in Tennessee grew 49 percent annually from 2010 to 2015, but in the same period contracted discounts, charity care and bad debt collectively grew by 61 percent annually. Policymakers need to pay attention to the growing financial constraints that many hospitals in rural areas across the country are facing.
In the Tennessee Delta, a Poor Community Loses its Hospital — and Sense of Security
The demise of Haywood Park Community Hospital in Brownsville nearly three years ago added to an epidemic of dying hospitals across rural America, according to the Washington Post. Nearly 80 have closed since 2010, including nine in Tennessee, more than in any state but Texas. Many more are considered fragile — downstream victims of federal health policies, shifts in medical practice and the limited tolerance of distant corporate owners for empty beds and financial losses.
2015 Tennessee State Health Plan
Tennessee’s State Health Plan released by the Department of Health offers a blueprint for improving the health of people in Tennessee. The work is centered around promoting the health of the public, access to healthcare, economic efficiencies, the quality of care and the workforce. For the first time, the State Health Plan now features an actionable repository of opportunities and recommendations that can be used by groups at all levels to improve health in their communities. The repository also includes best practices from across the state. Future State Health Plans will introduce measures similar to the National Academy of Medicine’s Vital Signs that the state can use to measure the progress.
Tennessee Medical Association: Hands off Tennessee’s Medical Liability System
A Georgia-based organization, Patients for Fair Compensation, is attempting to dismantle and replace Tennessee’s medical-liability system, according to The Tennessean. The Tennessee Medical Association claims Tennessee has one of the most favorable climates for medical liability in the country, which keeps the state competitive in retaining the best physicians. Further, that the civil legal system, hospital quality improvement committees, health plan utilization and medical necessity reviews, state and federal pilot initiatives, and the state licensing boards keep physicians accountable for legitimate injuries and quality of care. Tort reforms enacted since 2008 resulted in a 40 percent drop in volume of medical-liability claims filed against physicians and a 37 percent drop in physicians’ insurance premiums.
FTC Opposes Proposed Merger of Mountain States, Wellmont Health
The FTC recommended Tennessee regulators reject the proposed merger of two large regional health systems currently operating in several states including Tennessee, according to Modern Healthcare. FTC official Mark Seidman said the deal would cause an anticompetitive healthcare climate in the state, leading to higher prices and lower quality of care for patients, although the health systems claim the opposite.
Rural Tennessee Struggles with Changing Face of Healthcare
A slew of rural community hospitals in Tennessee are shutting down due to strained financing, according to the Knoxville News Sentinel. In states such as Tennessee where Medicaid eligibility has not been expanded to more income levels, rural hospitals are struggling because of a decrease in their federal reimbursement rates. Although at least eight rural Tennessee hospitals have closed or merged since 2013, five have been replaced by other satellite campuses of health systems or other clinics trying to fill the community's health services niche.
Brief History of Tennessee’s All-Payer Claims Database
After being enacted and implemented in 2009, Tennessee’s all-payer claims database (APCD) ceased operations in October 2011 when the contract with the original contractor lapsed, according to the Tennessee Department of Health Care and Financing (HCFA). The APCD was transferred to a newly-created HCFA, which procured a new ACPD vendor on Nov. 1, 2013. In 2015, all payers and insurers began submitting data again including, historical data since Jan. 1, 2012, and ongoing data on a prospective basis. By statute, the Tennessee Health Information Committee oversees and approves the data management, reporting, and research activities of the APCD and may impose penalties on payers that fail to comply with their obligations.
All-Payer Claims Databases: Initiatives to Improve Health Care Transparency
The Tennessee Department of Commerce and Insurance, Division of Health Planning plans on launching their APCD in 2010, according to the Commonwealth Fund. The goal is to use the data to improve healthcare access, affordability, and coverage; inform healthcare policy; determine the capacity and distribution of existing health care resources; evaluate the effectiveness of intervention programs to improve patient outcomes; compare costs across treatment setting and providers; and provide the public with information on healthcare quality.
Long-Term Care Legislation Enacted
The Long-Term Care Community Choices Act has been signed by the Governor, providing $1.2 billion to traditional nursing homes and community-based services providers in Tennessee’s managed care Medicaid program, according to the National Governors Association. The law provides consumers more choices for residential care providers and allows Medicaid funds to serve more people in cost-effective home and community settings.