Consumer-Centric Healthcare: Choosing a Doctor
Healthcare is increasingly touted as consumer- or patient-centered. Research is beginning to show that revealing and catering to consumer preferences can lead to better outcomes, more efficient spending and higher patient satisfaction. But our health system too often fails to provide what consumers really want and need.
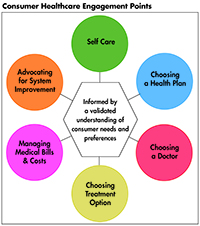
This Easy Explainer describes one of six consumer healthcare engagement points explored in the Hub’s Research Brief No. 18, Consumer-Centric Healthcare: Rhetoric vs. Reality, which outlines how these failings could be addressed and encourages a discussion of how to elevate, support and validate the consumer’s voice.
What are Consumers’ Preferences and Needs?
The relationship and interactions with one’s doctor or other healthcare provider remains the most important healthcare consideration for consumers.1 While the importance of relationships and interactions is true for all consumers, it was especially true for Hispanics and seniors; and Hispanic consumers found special importance in the relationships between their provider and family.2
When choosing a provider, consumers are interested in quality information that reflects elements of patient experience, such as bedside manner and service quality, such as follow-up care and personalized instructions.3 Consumers prefer doctors or other healthcare providers who spend time with them and do not rush; who listen and show they care about them; who clearly explain what they are doing and what the consumer needs to do later; and who provide clear, helpful information about the consumer’s diagnoses and conditions.4 When consumers are asked about “quality” of their healthcare, they often think about it in terms of the quality of their own provider: treatment is effective (77 percent), treats me well and with respect (74 percent), keeps me fully informed (71 percent), receive the care I expect (69 percent), and treats me as a person not a patient (69 percent).5
Convenience is important to consumers. Nearly two-thirds of consumers say they would switch providers for the ability to get an appointment quickly when they need it; and more than half would also switch for the ability to get an appointment at a convenient location.6 Language is a key provider attribute for Spanish speakers.7 Spanish speakers often find it hard to communicate with doctors.8
To choose a doctor, most consumers (74 percent) continue to rely on opinions and recommendations of friends and relatives.9
Many will also use computer searches as a starting point, but lower-income consumers often don’t know the precise search terms to use.10 Many low-income consumers perform searches for indicators that a physician will be respectful, often using the physician’s photograph as a proxy.11
Consumers report they are most interested in information that reflects elements of the patient experience or service quality. However, only about one-in-four (27 percent) have used online ratings of a doctor’s bedside manner or wait time; only 22 percent looked at online ratings of clinical quality to help them decide on a medical provider; and few consumers (14 percent) used data on the cost of care to select a doctor.12
Focus groups reveal that consumers don’t realize that the quality of healthcare can vary among providers and that may be the reason that clinical proficiency isn’t listed more often among their stated preferences.13 Consumers assumed that some “watch dog” was ensuring that poor performers were kept from practicing.
How the System Fails Consumers
Consumers are not aware of independent, trusted sources of information that they can use to choose among providers that matches their preferences for information on bedside manner, convenience and language. While quality reports capture elements that resonate with experts and healthcare professionals (mortality rates, clinical quality measures), consumers often are more interested in quality information that reflects elements of the patient experience or service quality.
Moreover, patient experience surveys-which could help inform consumers when they are searching for a physician-have been used primarily with Medicare and privately insured populations, leaving the voices of patients in the lowest socioeconomic status underrepresented.14
And information is not geared to consumer preferences. For quality and cost information to be meaningful to consumers, it needs to reflect consumer priorities and be presented in a way that makes it accessible and understandable. Even highly motivated consumers are likely to abandon efforts to find information if difficult to find or understand.
Spanish speakers often struggle with language barriers when it comes to understanding insurance terms or in communicating with providers. They often don’t ask for resources, even when available, for fear of prejudice against immigrants.
Failure to keep poor performers from practicing. Consumers want to know they can navigate their physician choices safely, without encountering a physician who has lost their license in a nearby state. While rare, it is still too common that physicians’ reputations are protected at the expense of patients.15
How the System Can Better Meet Consumers’ Preferences and Needs
Build the healthcare workforce consumers are looking for by providing training and support to physicians and other providers to better communicate with and understand consumer preferences and needs, and practice shared-decision-making.16 Hiring a more diverse workforce, making language access a high priority, and even something simple like making more eye contact could greatly improve trust and respect in provider-patient relationships and interactions.
Provide comparative quality information geared to consumers’ preferences and make the information easier for consumers to find and use. And remove one consumer choice burden by doing a better job of prohibiting dangerous doctors from practicing.
Make it mobile. Vulnerable consumers use mobile phones for 90 to 95 percent of their internet use, including to access health information.17
Notes
1. Findings from Deloitte’s 2016 Consumer Priorities in Healthcare Survey, Deloitte (2016).
2. Ibid.
3. Sick, Brian, and Jean M. Abraham, “Seek and Ye Shall Find – Consumer Search for Objective Healthcare Cost and Quality Information,” American Journal of Medical Quality, Vol. 26, Issue 6 (Sept. 14, 2011).
4. Ibid.
5. Novant Health-Harris Poll (March 30, 2016).
6. Collier, Matthew, and Leslie Meyer Basham, Patient Loyalty: It’s Up For Grabs, Accenture (2016).
7. Saha, Sommath, et al., “Do Patients Choose Physicians of Their Own Race,” Health Affairs, Vol. 19, No.4 (July 2000).
8. Ibid.
9. Lynch, Wendy, Kristen Perosino, and Michael Slover, Altarum Institute Survey of Consumer Health Care Opinions, Altarum Institute (Spring 2014).
10. Ibid.
11. Ibid.
12. Lynch, Wendy, Kristen Perosino, and Michael Slover (Spring 2014).
13. Consumers Union, Engaging Consumers on Health Care Cost and Value Issues. (October 2014).
14. Browne, Katherine et al., “Measuring Patient Experience as a Strategy for Improving Primary Care,” Health Affairs, Vol. 29, No. 5 (May 2010).
15. Peachman, Rachel, What You Don’t Know About Your Doctor Could Hurt You, Consumer Reports (April 20, 2016).
16. Coulter, Angela, and Alf Collins, Making Shared Decision-Making A Reality: No Decision About Me, Without Me, The King’s Fund (2011).
17. Leis, Helen, Parie Garg, and Iueh Soh, Right Place, Right Time: Marketplace Responses to the Health Information Needs of Vulnerable Consumers, Oliver-Wyman, Altarum Institute, Robert Wood Johnson Foundation (January 2017).