Consumer-Centric Healthcare: Seeking Self Care
Healthcare is increasingly touted as consumer- or patient-centered. Research is beginning to show that revealing and catering to consumer preferences can lead to better outcomes, more efficient spending and higher patient satisfaction. But our health system too often fails to provide what consumers really want and need.
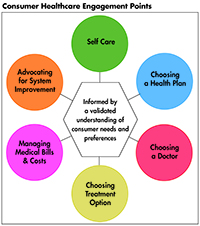
This Easy Explainer describes one of six consumer healthcare engagement points explored in the Hub’s Research Brief No. 18, Consumer-Centric Healthcare: Rhetoric vs. Reality, which outlines how these failings could be addressed and encourages a discussion of how to elevate, support and validate the consumer’s voice.
What are Consumers’ Preferences and Needs?
For healthy individuals, self care includes eating a balanced diet, exercising regularly, getting adequate sleep, and avoiding high-risk behaviors such as smoking. Americans clearly understand the importance of being healthy and overwhelmingly aspire to lead healthy lives.1,2 They feel that they are responsible for staying healthy and that their personal lifestyle choices matter.3
But what consumers aspire to and what they actually do are two different things. For example, 89 percent say taking personal responsibility for one’s health is the best way to stay healthy, 75 percent say they feel they can manage health issues through nutrition, and 64 percent say they will take whatever means necessary to control their own health. However, when it comes to action, only 70 percent say they are actively trying to be healthier, 50 percent say it’s a challenge to eat healthy and 66 percent say they don’t exercise enough.4 These statistics show the difference between stated preferences and revealed preferences.
Nearly all U.S. adults in a recent poll expressed concerns that something was interfering and keeping them from being as healthy as they could be. Three quarters of American adults say there is some barrier to being their healthiest self. Most commonly, these barriers are lack of interest/motivation, time, cost, and competing responsibilities.5
If becoming active in one’s health is hard for healthy individuals, it becomes even more difficult when an individual becomes critically ill or injured.6 For example, the potential scope of self-care activities after hospital discharge could include taking prescribed medications, sampling and interpreting one’s own blood or urinary laboratory values, changing dressings, administering parenteral nutrition, monitoring and adjusting fluid and dietary intake and output, and suctioning one’s airway.7
Although studies suggest that self-care can lead to cost savings and better outcomes in the prevention and treatment of asthma,8 chronic obstructive pulmonary disease,9 diabetes,10 and other chronic conditions,11 a key question is how far people are able to participate in their own healthcare? While some people are very proactive about their health, many are quite passive or face barriers to self-care.
How Our System Fails Consumers
Social, political, economic and environmental barriers have been identified that inhibit consumers trying to lead healthy lives and exercise personal responsibility.
Studies have shown that consumers are highly responsive to even subtle environmental cues,12 so large shifts in access, pricing, portion sizes, marketing, and other powerful drivers of eating and physical activity will have major effects on weight and fitness.
Progress is slowed by he fact that we don’t have consensus on the right balance between personal responsibility and the role of public “nudges” (or even stronger measures). Policymakers may frame certain public health issues as either an individual responsibility or as an environmental issue resulting in very different policy recommendations.13 If getting to good health outcomes is the goal, we must not let the framework of personal responsibility use blame, bias, stigma, and discrimination to avoid regulatory or governmental action that would provide necessary supports and interventions that would help Americans to better achieve their aspirations for living healthy lives.14
Moreover, when trying to support and incentivize consumers, one-size-fits-none. Providers, health plans, government officials, consumers, and others need to acknowledge that some people are less likely to be active in their self-care15 and face varying levels of structural barriers to self-care. If a patient feels overwhelmed, has little confidence, and has had experience of failing to manage their health, it can be overwhelming when a doctor tells them that, because of a new diagnosis, they need to make multiple changes to their lifestyle—changing their diet, increasing their physical activity and managing new medications. They may try to make these changes, but when they cannot make all of them, they will most likely make none. By not understanding that a patient like this has limited self-care skills, their doctor has set them up for failure.16
How the System Can Better Meet Consumers’ Preferences and Needs
The priority must be on additional research to identify and address the social, political, economic and environmental barriers to self-care. With a robust understanding of these barriers, policymakers must then address the challenges of balancing personal and environmental approaches to serve the greater public good, e.g., smoking reductions, the use of seat belts, wearing a bike helmet, clean air and safe drinking water. A nuanced use of behavioral economics, social cues and guidance may help improve results.
Providers can help patients identify personal preferences and goals for self-care and barriers that inhibit realizing goals. For some patients, identifying community and employer resources that might address barriers and proven techniques for promoting self care can improve health outcomes. Health plans should pay for, and health systems should encourage, longer appointments for patients with greater need, and all stakeholders should guide investments in local, community-based support services.17
Measuring patient activation levels would help health providers target time and resources to patients.18 We can maximize the value of doctor’s appointments for less-activated patients by using specially trained medical assistants, such as health coaches, to meet the patient prior to their appointment to help them formulate their self-care questions for the clinician.19
1. Novant Health-Harris Poll, Consumer Attitudes about Health Study, Winston–Salem, N.C. (March 30, 2016).
2. Nielson Company and NMI, Health & Wellness in America 2014 (2014).
3. Novant Health-Harris Poll, Consumer Attitudes about Health Study, Winston–Salem, N.C. (March 30, 2016).
4. Nielson Company and NMI, Health & Wellness in America 2014 (2014).
5. Novant Health-Harris Poll, Consumer Attitudes about Health Study, Winston–Salem, N.C. (March 30, 2016).
6. Alspach, JoAnn Griff., “The Patient’s Capacity for Self-Care: Advocating for a Predischarge Assessment,” Critical Care Nurse, Vol. 31 No. 2 (April 2011).
7. Ibid
8. Lahdensuo, Aarne, et al., “Randomized comparison of Cost Effectiveness of Guided Self management and Traditional Treatment of Asthma in Finland,” BMJ, Vol .316, No. 1138 (1998).
9. Gallefoss, Frode, and Per S. Bakke, “Cost-Benefit and cost-effectiveness Analysis of Self-Management in Patients with COPD – A 1-year Follow-up Randomized, Controlled Trial,” Respiratory Medicine, Vol 424, No. 31 (July 2002).
10. Li, Rui., et al., “ Cost-Effectiveness of Interventions to Prevent and Control Diabetes mellitus: A Systematic Review,” Diabetes Care, Vol. 33, No. 8 (August 2010).
11. Kennedy, Anne., et al., “ The Effective and Cost-Effectiveness of a National Lay-Led Self Care Support Programme for Patients with Long-Term Conditions: A Pragmatic Randomised Controlled Trial,” Journal of Epidemiology & Community Health, Vol.61, Issue 3 (2001).
12. Brownell, Kelly D., et al., “Personal Responsibility and Obesity: A Constructive Approach to a Controversial Issue,” Health Affairs, Vol. 29, No. 3 (March 2010).
13. Ibid.
14. Ibid.
16. Hibbard, Judith, and Peter J. Cunningham, How Engaged are Consumers in Their Health and Healthcare, and Why does it Matter?, Center for Studying Health System Change. Washington, D.C. (October 2008).
17. Hibbard, Judith, and Helen Gilburt, Supporting People to Manage Their Health: An Introduction to Patient Activation, The King’s Fund, London, U.K. (May 2014).
18. National Health Service England, How Much do Clinicians Support Patient Activation?, London, U.K. (November 20, 2015).
19. Hibbard, Judith, and Helen Gilburt. (May 2014).
20. Ibid.