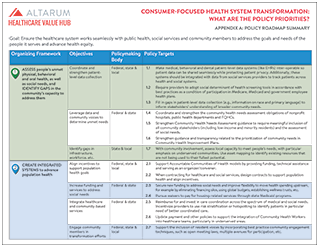
Consumer-Focused Health System Transformation:
What are the Policy Priorities?
Appendix A: Policy Roadmap Summary
Goal: Ensure the healthcare system works seamlessly with public health, social services and community members to address the goals and needs of the people it serves and advance health equity.
|
Organizing Framework |
Objectives |
Policymaking Body |
Policy Targets |
|
|
ASSESS people’s unmet physical, behavioral and oral health, as well as social needs, and IDENTIFY GAPS in the community’s capacity to address them |
Coordinate and strengthen patient-level data collection |
Federal, state & local |
1.1 |
Make medical, behavioral and dental patient-level data systems (like EHRs) inter-operable so patient data can be shared seamlessly while protecting patient privacy. Additionally, these systems should be integrated with data from social services providers to track patients across health and social systems. |
|
1.2 |
Require providers to adopt social determinant of health screening tools in accordance with best practices as a condition of participation in Medicare, Medicaid and government employee health plans. |
|||
|
1.3 |
Fill in gaps in patient-level data collection (e.g., information on race and primary language) to inform stakeholders’ understanding of broader community needs. |
|||
|
Leverage data and community voices to determine unmet needs |
Federal & state |
1.4 |
Coordinate and strengthen the community health needs assessment obligations of nonprofit hospitals, public health departments and FQHCs. |
|
|
1.5 |
Strengthen Community Health Needs Assessment guidance to require meaningful inclusion of all community stakeholders (including low-income and minority residents) and the assessment of social needs. |
|||
|
1.6 |
Strengthen guidance and transparency related to the prioritization of community needs in Community Health Improvement Plans. |
|||
|
Identify gaps in infrastructure, workforce, etc. |
State & local |
1.7 |
With community involvement, assess local capacity to meet people’s needs, with particular emphasis on underserved communities. Use asset mapping to identify existing resources that are not being used to their fullest potential. |
|
|
CREATE INTEGRATED SYSTEMS to advance population health |
Align incentives to support population health goals |
Federal, state & local |
2.1 |
Support Accountable Communities of Health models by providing funding, technical assistance and serving as an organizer/convener. |
|
2.2 |
When contracting for healthcare and social services, design contracts to support population health and align incentives. |
|||
|
Increase funding and services to address social needs |
Federal & state |
2.3 |
Secure new funding to address social needs and improve flexibility to move health spending upstream, for example by eliminating financing silos, using global budgets, establishing wellness trusts, etc. |
|
|
2.4 |
Pursue waivers to pay for housing-related services through state Medicaid programs. |
|||
|
Integrate healthcare and community-based services |
Federal & state |
2.5 |
Reimburse for and invest in care coordination across the spectrum of medical and social needs. Incentivize providers to use risk stratification or hotspotting to identify patients in particular need of better coordinated care. |
|
|
2.6 |
Update payment and other policies to support the integration of Community Health Workers into healthcare teams, particularly in underserved areas. |
|||
|
Engage community members in transformation efforts |
Federal, state & local |
2.7 |
Support the inclusion of resident voices by incorporating best practice community engagement techniques, such as open meeting laws, multiple avenues for participation, etc. |
|
|
ENSURE MEANINGFUL ACCESS to care and services that meet people’s goals and needs, especially within underserved communities |
Provide universal, comprehensive coverage |
Federal, state & local |
3.1 |
Adopt one of several possible evidence-based universal coverage policies. Ensure covered benefits are comprehensive; premiums and cost-sharing are tailored to family means; and eligibility criteria (if present) are as simple as possible and designed to enhance population health. Similarly, design provider networks to reflect community goals and needs. |
|
Address provider shortages; increase diversity among providers |
Federal & state |
3.2 |
Expand scholarships, federal and state loan repayment programs and other incentives for physicians and mid-level providers to practice in underserved areas and recruit those from under-represented (i.e. minority) groups. Similarly, invest in “pipeline” programs to recruit providers likely to practice in underserved areas, as well as those from under-represented groups. |
|
|
3.3 |
Increase reimbursement for primary care (broadly defined). |
|||
|
3.4 |
Broaden non-physician providers’ “scope of practice” and/or create new categories of medical and dental providers with expanded authority. |
|||
|
Tailor care delivery settings to community needs |
Federal & state |
3.5 |
Improve access by co-locating primary care, behavioral health and oral health facilities. Eliminate regulatory barriers preventing payment for same-day services from FQHCs, behavioral health and dental service providers. |
|
|
3.6 |
Support a transition from traditional, hospital-based care to alternative settings that better meet patients’ needs by increasing flexibility for critical access hospitals with respect to the services they provide. |
|||
|
3.7 |
Expanding use of and reimbursement for telemedicine. |
|||
|
Make clinical care more patient-centered |
Federal, state & local |
3.8 |
Require clinicians to use shared decision-making to surface patients’ goals, needs and preferences as a condition of participation in Medicare, Medicaid and government employee health plans. |
|
|
3.9 |
Develop standards for and require providers to undergo anti-oppression and equity training as a condition of participation in government-sponsored coverage. |
|||
|
3.10 |
Expand the use of patient and family advisory councils to amplify the consumer voice in governance decisions. Provide adequate training and support, when necessary, to ensure that a diversity of community members can participate effectively. |
|||
|
Use measurement and feedback systems to judge performance |
Federal, state & local |
3.11 |
Use a multi-stakeholder process to determine how overall success will be measured, develop new measures as needed and ensure meaningful feedback mechanisms to evaluate progress. |
|