Improving Value
Addressing Low Value Care
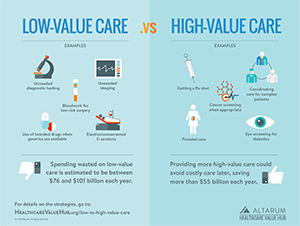
A shocking amount of healthcare is considered unnecessary. Across several large studies, it is estimated that 3% or more of total healthcare spending was for unneeded services or due to delivery inefficiencies (for example, test results not being shared).1 Services that have been identified as low- or no-value number more than 500, according to the Choosing Wisely campaign.2 Examples include:
- An EEG for a patient with a headache, or a CT scan or MRI for a patient with lower-back pain and no signs of a neurological problem
- Emergency room visits for non-emergencies
- Surgery when physical therapy would be equally or more effective
- Inappropriately prescribed antibiotics
Examining just a handful of these low-value services, researchers have studied the prevalence of low-value care in the Medicare, commercial and Medicaid populations (adults and children) and found that high rates of overuse are very localized. After controlling for locality, rates of overuse do not vary significantly by insurance type.
Reducing the Provision of Low-Value Care
Purchasers, providers, patients and policymakers all have key roles to play in reducing the provision of low- and no-value care.3
As a starting point, the U.S. must increase funding for Comparative Effectiveness Research to clarify which treatments work best — and for which types of patients. It has been estimated that half of the treatments delivered do not have clear evidence of effectiveness.
Beyond that, the localized nature of overuse suggests that payer or state strategies to identify where low-value services are being provided is a key initial strategy, so that subsequent efforts are well targeted. Broadly speaking, these approaches include:
- gaining consensus around the list of low-value services,
- provide accurate information to both physicians and patients regarding the risks of these services, and
- consider financial and non-financial incentives for providers and patients to discourage their use.
The Hub's issue brief, Reducing Low-Value Care: Saving Money and Improving Health, provides examples of low-value care services and walks readers through the strategies to address low-value care, including:
- shifting away from traditional fee-for-service payment approaches and towards those that pay for performance rather than volume;
- encouraing integrated care through models such as Accountable Care Organizations (ACOS); and
- sending usable signals to patients via Value-Based Insurance Design (VBID) (Note: VBID has traditionally lowered the patient's cost-sharing requirements in order to encourage the consumption of high-value care. Largely untested is whether raising cost-sharing requirements for services that are considered low-value is needed to reduce the use of these services. It may be more effective to work directly with providers to ensure that low-value services aren't even recommended in the first place.)
"Clinician Focused Awareness Campaigns" and "Patient Awareness" strategies are other strategies explored in the brief. Authors find evidence around the strategies to reduce low-value care is fairly strong, particularly when the strategies are deployed as part multicomponent initiatives that align financial and non-financial incentives for providers and patients.
In addition to the actions that payers and purchasers can take, there are steps states can take, including:
- prioritizing the reduction of low-value care;
- building a culture of trust, innovation and improvement;
- establishing a shared language and purpose; and
- committing resources to measurement.
ExampleThe nonprofit Virginia Center for Health Innovation (VCHI) analyzed claims data and found that providers in the state ordered 5.4 million services that were considered low-value, resulting in over $586 million, or $9.09 per beneficiary per month, in wasteful spending in 2015.4 Subsequently, the VCHI received a $2.2 million grant from Arnold Ventures to create a statewide pilot aimed at reducing the provision of low-value care. The pilot will create a large scale health system learning community and an employer task force on low-value healthcare. A latter part of the project will develop a set consumer-driven measures. |
Notes
1. Hunt, Amanda, "Six Categories of Healthcare Waste: Which Reign Supreme?" Healthcare Value Hub blog (October 2019).
2. While not the only source for identifying low-value care, the American Board of Internal Medicine (ABIM) Foundation's Choosing Wisely initiative is one of the most widely recognized. The campaign aggregates recommendations from industry experts on how to reduce low-value care and distributes that information to clinicians and patients. Other efforts to identify low-value care include the U.S. Preventive Services Task Force (services rated "D") and the National Institute for Health and Care Excellence ("do not do" recommendations) in the UK. Low-value care has also been identified in Health Assessments performed by the Canadian Agency for Drugs and Technologies and various peer-reviewed medical journals.
3. Buxbaum, Jason D., et al., "Tackling Low-Value Care: A New 'Top Five' for Purchaser Action," Health Affairs (November 2017).
4. LaPointe, Jacqueline, "Low-Cost, Low-Value Resource Use Drives $586M in Wasteful Spending," RevCycleIntelligence (October 2017).
- BMC Health Services Research: Are Low-Value Care Measures Up To the Task? A Systematic Review of the Literature (August 18, 2016).
- JAMA: Measuring Low-Value Care in Medicare (July 2014).
- Journal of General Internal Medicine: Choosing Wisely: Prevalence and Correlates of Low-Value Health Care Services in the United States (February 2015).
- Sage Journals: Interventions Aimed at Reducing Use of Low-Value Health Services: A Systemic Review (July 8, 2016).
- Oxford Academic International Journal for Quality in Health Care: Limit, Lean or Listen? A Typology of Low-Value Care That Gives Direction in De-Implementation (May 7, 2018).
- BMC Health Services Research: Exploring Variation in Low-Value Care: A Multilevel Modelling Study (May 30, 2019).