State News
Connecticut
Connecticut has explored many approaches to improving healthcare value for consumers over the past several years. The state created an all-payer claims database in 2012 and passed a comprehensive law prohibiting certain out-of-network billing practices and establishing a “certificate of need” process for insurance companies to acquire physician groups in 2015. The law also requires health insurance companies to submit an annual report to the Connecticut Health Insurance Exchange that lists the billed and allowed amounts paid to each healthcare provider in the insurer’s network for certain diagnoses and procedures, and the corresponding out-of-pocket costs. The state launched an Office of Health Strategy in 2018 to implement comprehensive, data-driven strategies that promote equal access to high-quality healthcare, control costs and ensure better health for Connecticut residents. Among other responsibilities, the office will oversee the state’s four-year State Innovation Model grant to test multi-payer healthcare payment and service delivery models to improve health system performance, increase quality of care and decrease costs.
As of 2019, Connecticut was one of the few states that has comprehensive protections from surprise medical bills. However, high drug costs remain a significant consumer concern. The state has passed several pieces of drug pricing legislation to address these concerns, including laws that require pharmaceutical companies to disclose and explain drug price hikes; force pharmacy benefit managers to report how much they collect in rebates and how much they keep; and protect pharmacists from “gag clauses” that prohibit them from disclosing specified information to people purchasing certain drugs.
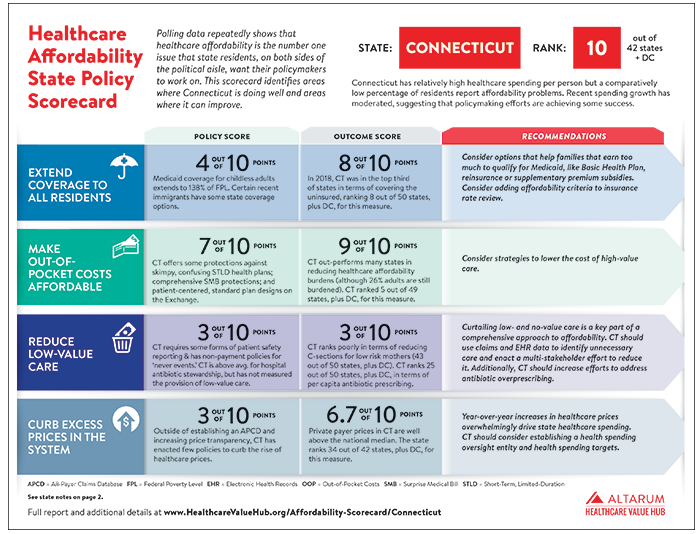
Connecticut ranked 11 out of 47 states plus DC, with a score of 46.1 out of 80 possible points in the Hub's 2021 Healthcare Affordability State Policy Scorecard.
Connecticut Modifying 2024 Health Cost Growth Benchmark Due to High Inflation
Connecticut will be raising the cost growth benchmark target to four percent due to high inflation,
reports the state Office of Health Strategy. In consultation with health system stakeholders and
experts, OHS had previously established Connecticut's benchmarks at 3.4 percent for 2021, 3.2
percent for 2022, and 2.9 percent for 2023, 2024, and 2025. Notably, the statewide per-person
spending for 2020-2021 exceeded the 3.4 percent benchmark, with a 6 percent increase in
overall per-person spending statewide.
Connecticut to Remove Medical Debt for Thousands Across the State
Connecticut will become the first state to use American Rescue Plan Funding to forgive medical
debt among residents, reports New Hampshire Public Radio. Last year, state policymakers
allocated $6.5 million in the state budget towards erasing eligible residents' medical debt and
over the next several months, Connecticut will collaborate with a nonprofit that purchases
medical debt at a reduced rate to begin the process. Eligibility for relief extends to state
residents whose medical debt exceeds five percent of their income or who earn up to four times
the federal poverty line. Notification for eligible individuals could occur as early as this summer,
according to the governor’s office.
In Three States, Growth in Prescription Drug Spending Is Unaffordable Even When Accounting for Rebates
Data from Connecticut, Rhode Island, and Oregon shows that even after accounting for rebates,
spending on prescription drugs has continued to grow at an unaffordable rate, according to
Health Affairs Forefront. Connecticut, Rhode Island, and Oregon collect aggregate spending
data from payers as part of their cost growth targets and found that accounting for prescription
drug rebates did not lower spending growth to an affordable level, relative to household income
level, in the commercial market. Between 2018 and 2021, average retail prescription drug
spending in these states grew between 6.0 percent and 9.2 percent; accounting for rebates
reduced spending growth to between 3.2 percent and 6.1 percent during this time period.
Connecticut Launches State Prescription Drug Card
Connecticut residents, regardless of immigration status, now have access to a state-run
prescription drug discount card, reports NHPR. Beginning October 2, 2023, residents can sign
up for a free ArrayRx discount card that can be used at about 98 percent of pharmacies in the
state. All FDA-approved drugs are eligible for a discount, and it is estimated that the discount
card will decrease the costs of generic medications by upwards of 80 percent.
Connecticut Deploys Paraeducator Health Insurance Fund
Connecticut has announced the creation of a subsidy program designed to decrease annual
out-of-pocket health care costs for paraeducators across the state, reports the CT Mirror. The
subsidy is expected to pay up to 74 percent of the paraeducators' annual out-of-pocket health
care costs, and it is estimated that about 4,166 paraeducators will receive some amount of aid.
The stipend is a long-awaited relief for the 73 percent of paraeducators with high deductible
health plans who have been struggling to pay for their health care bills.
Analysis of Pandemic Telehealth Use in Connecticut Released
Telehealth appointments, costs, ER visits and hospitalizations among privately insured patients
increased significantly in Connecticut from 2020-2022, reports the CT Mirror. The study did not
determine whether these increases were necessary or unnecessary, or whether there was a
causal relationship between telehealth services and the measured results. However, the
research did find that greater racial and ethnic diversity in an area was correlated with a higher
average number of ER visits and hospitalizations among patients who use telehealth and those
who do not use it, indicating a need for greater efforts to diminish health inequities in the state.
Study Finds Mortality Rate Higher for Connecticut’s Black Population
Connecticut's Black population has a higher mortality rate than its white population, reports
WSHU. The report found that Black infants are three times more likely to die than white infants
in the state. Furthermore, between 2017 and 2022, Black residents were much more likely to die
from preventable illnesses like COVID-19, kidney disease, and heart disease. The report
suggests that discrimination in health care settings, poor housing, financial and food insecurity,
and other upstream factors contribute to higher mortality rates among Black residents.
Governor Signs Legislation on Health Care Affordability
Connecticut’s Governor signed legislation designed to address the rising costs of health care in the state, reports the State Department of Public Health. The law (HB 6669) includes a drug discount card program for all residents, stricter oversight of prescription drug marketing, updated annual drug reporting requirement thresholds to ensure enhanced scrutiny of costs, expanded prohibitions on facility fees, increased competition in health care markets, and improved Certificate of Need protocols. Additionally, the legislation mandates various studies on affordability-related topics be conducted in the upcoming years.
Connecticut Budget Includes Provisions to Erase Millions in Medical Debt
Connecticut’s budget includes provisions to eliminate medical debt for Connecticut families, reports the CT Insider. The plan involves collaborating with nonprofit organizations that negotiate with hospitals to purchase medical debt at significant discounts and subsequently cancel it. The budget allocates $6.5 million, which legislators believe can erase hundreds of millions of dollars in medical debt.
Connecticut and Pennsylvania Pursue Maternity-Focused Value-Based Payment Models
Connecticut and Pennsylvania have developed value-based payment models for Medicaid providers that are focused on maternity care, according to the NASHP. Connecticut uses a voluntary pay-for-performance model where providers are eligible for bonus payments if certain quality metrics are met, including receipt of a comprehensive postpartum visit, self-measured blood pressure, and low-dose aspiring for certain patients. Pennsylvania uses a bundled payment where providers receive bonus payments determined by quality metrics, such as postpartum depression screenings and follow-up, substance use disorder treatment, and well-child visits, as well as decreased cost of care. To address racial disparities in maternal mortality, providers that meet these metrics for Black patients in Medicaid can receive additional incentives.
Connecticut Expands Coverage to a Greater Number of Immigrant Children; Funds Community Health Workers through Medicaid
Connecticut has implemented significant changes to its Medicaid program, reports the Connecticut Mirror. During the most recent legislative session, the state: expanded Medicaid coverage eligibility to undocumented children fifteen years of age and younger; increased the income limit to qualify for HUSKY part C for the elderly, blind, and disabled to 105% of FPL; and will require the Department of Social Services to design and implement Medicaid reimbursement policies to compensate community health workers.
Connecticut Health Care Spending Outpaces Economic Growth, Exceeds Cost Growth Benchmark
Health care spending in Connecticut has eclipsed economic growth in recent years, according to Connecticut Public Radio. Spending increased 6 percent between 2020 and 2021, which exceeded the state benchmark target of 3.4 percent, and was driven primarily by increases in commercial health insurance spending.
Governor Announces Agreement to Expand Access to Health Coverage for Personal Care Attendants
Connecticut is expanding affordable access to health coverage for personal care attendants (PCAs), according to the Office of Governor Greg Lamont. PCAs provide vital care for individuals with disabilities and chronic illnesses, but many do not have access to affordable health insurance. Under the agreement between the state government, advocates for individuals with disabilities, and health insurance providers,
PCAs will be able to enroll in the state’s health insurance exchange and receive subsidies to help pay for their premiums. This will provide access to comprehensive health coverage for thousands of PCAs who currently lack insurance.
Connecticut Hospitals Spend Less Than National Average on Financial Assistance
Two in ten Connecticut residents insured through the state's health insurance marketplace struggle to afford necessities due to health care costs, according to the Hartford Courant. Despite the burden of medical debt across the state, area hospitals spend less than the national average on financial assistance programs to support disadvantaged communities.
Connecticut Receives Federal Funding to Support Covered Connecticut Health Program
Connecticut has received federal approval for a Section 1115 demonstration waiver that will support the Covered Connecticut program, reports the Connecticut Office of Governor Ned Lamont. The approval provides federal matching funds to sustain the existing program, which offers federal premium subsidies, cost-sharing reductions and eliminates out-of-pocket costs for enrollees.
78 Percent of CT Residents Worried about Healthcare Affordability
Nearly four in five Connecticut residents are concerned about healthcare affordability, reports the Connecticut Mirror. In addition to this statistic, the survey also demonstrated that, among those surveyed, the issue of affordability extends across the political aisle—68 percent of Republicans, 75 percent of Democrats and 67 percent of residents who identified as neither party agreed the healthcare system needed change.
More than Half of Connecticut Residents with Private Insurance had a High Deductible Health Plan in 2020
More than half of Connecticut residents with private insurance are enrolled in a high deductible health plan, according to the Connecticut News Junkie. Patients covered by high deductible plans are one-third times more likely to have medical debt, and their debts average $4,000 higher, than people without high deductibles. Medical debt impacts Connecticut residents across the socioeconomic demographic—the Hartford Foundation for Public Giving, which operates a charity fund for individuals struggling with medical debt in the state, reports that the majority of their applicants receive insurance coverage through their employer but are underinsured at the time of receiving care.
Access to Affordable Health Insurance Remains Elusive for Farmers
Nearly 30 percent of farmers, surveyed by the New Connecticut Farmers Alliance, describe their health insurance as “unaffordable” or “very unaffordable,” reports Connecticut Public Radio. The article also explains that only 5 percent of farmers or farm workers surveyed in Connecticut receive health insurance through their employer. The challenges surrounding affordable health insurance negatively impact health outcomes and financial security, discourages potential farmers from pursuing the profession and may lead to underinsurance in the population.
Connecticut Announces New Findings from Connecticut Healthcare Affordability Index
A report from the Office of Health Strategy and the Office of the State Comptroller focuses on the Connecticut Healthcare Affordability Index (CHAI), which measures the impact of policy models on Connecticut families’ ability to make ends meet. The findings measured the impacts of the cost of basic needs, income inadequacy rates and affordable healthcare rates by using the following policy models: American Rescue Plan (ARPA) Premium Tax Credit, Covered Connecticut and the Cost Growth Benchmark. The model estimates that if the temporary ARPA provision was available in 2019, nearly 31,000 additional households would have had affordable healthcare. It also estimates that expanding eligibility of the Covered Connecticut Program helped more than 17,000 additional households attain affordable coverage. Finally, by tying the rate of hospital spending growth to the cost growth benchmark, the model estimates that 14,000 additional households would attain affordable healthcare.
As Hospital Systems Grow in Connecticut, Rural Patients Lose Services
In Connecticut, two health systems are on the brink of owning more than half of the 27 hospitals in the state, reports the CT Mirror. In 2000, the state had 23 independent hospitals, but now it just has 6. Residents of Windham say that when their hospital was acquired by Hartford HealthCare, they were told they would get new services and highly trained specialists. But soon after, the critical care unit was converted to progressive care, which can’t handle the same complexity of care. Now, the health system is moving forward with plans to close the hospital’s labor and delivery unit, which is directly contradictory to promises made to the community. Cuts such as these have devastating impact on the state’s rural labor and delivery landscape.
Saint Francis Sues Hartford HealthCare, Claims Anti-Competitive Practices
Saint Francis Hospital and Medical Center has sued Hartford HealthCare and its subsidiaries, reports the CT Mirror, claiming that it is trying to create a monopoly on hospital services by acquiring physician networks, particularly cardiologists, and demanding that they refer their patients only to Hartford HealthCare. The lawsuit alleges "a campaign of exclusion, acquisition and intimidation," and claims that Hartford HealthCare executives have stated in meetings that their plan was to "crush" or "bury" Saint Francis. The lawsuit also claims that as Hartford HealthCare acquired physician practices, it threatened and intimidated physicians who don't comply with its dictates. Hartford HealthCare has been cornering the market on lucrative operations such as cardiac and orthopedic surgeries by forcng doctors to send their patients only to Hartford HealthCare hospitals or by obtaining exclusive rights to robotic equipment.
Saint Francis Sues Hartford HealthCare, Claims Anti-Competitive Practices
Saint Francis Hospital and Medical Center has sued Hartford HealthCare and its subsidiaries, including Hartford Hospital, reports CT Mirror. Saint Francis claims that Hartford HealthCare is trying to create a monopoly on hospital services by acquiring physician networks, particularly cardiologists, and demanding that they refer patients only to Hartford HealthCare. The lawsuit claims that as Hartford HealthCare acquired physician practices, they threatened and intimidated physicians who don’t comply with its “dictates.” The lawsuit also claims that other hospitals in the region suffer due to Hartford HealthCare’s “anticompetitive conduct.”
With Medical Bills Soaring, Nonprofits, Crowdfunding, Payment Plans Offer Some Debt Relief
Lori Dingwell of Waterbury, Connecticut, tested positive for COVID-19 in February 2021 and, though she has seen numerous specialists, has yet to fully recover, reports Connecticut Health I-Team. Suffering from long-haul COVID, Dingwell has racked up nearly $10,000 in medical debt and is paying out-of-pocket for her mental healthcare, as well as a large share of her medical treatment, though she has health insurance through the state's exchange. Dingwell does not qualify for Medicaid, though she is low-income, and Connecticut ranks among the highest in the country for per capita spending on healthcare, yet medical debt remains an issue for consumers. When Dingwell was referred to a COVID clinic, the staff informed her that she would have to pay for the majority of her treatment out-of-pocket; Dingwell gave up.
Study Analyzes Effect of Connecticut 2016 Surprise Billing Law on Emergency Physician Services Market
A study by USC Brookings Schaeffer Initiative for Health Policy reveals preliminary evidence concerning Connecticut's 2016 Surprise Billing Law, reports AboutHealthTransparency.org. The law requires that a patient’s out-of-pocket costs be no greater than their in-network cost-sharing amounts if they are unknowingly treated by an out-of-network provider at an in-network facility. Researchers observed a stark and sudden increase in allowed amounts for fully insured plans within the state, coinciding directly with the implementation of the law. These findings suggest that the law, by pegging the minimum out-of-network payment requirement to the 80th percentile of provider charges, may have driven a substantial increase in allowed amounts paid to emergency physicians from fully insured plans. These increased allowed amounts are likely to be passed to consumers in the form of higher premiums.
Covered CT Program Offers Affordable Healthcare for All Residents
This summer, Connecticut launched a new Covered CT Program, which aims to reduce the number of residents who are uninsured by helping them afford insurance, reports Fox 61 News. The program is going to provide no-cost health coverage to up to 40,000 people in Connecticut when it’s fully implemented in 2022. In this new program, the state will pay the consumer portion of the monthly premium directly to insurance carriers and will also pay for the cost-sharing amounts that consumers normally would have to pay with a health insurance plan. Beginning in 2022, this program will also include coverage for visiting the dentist and non-emergency medical transportation to see providers.
Connecticut Governor Signs Bill Limiting Hospital Billing and Collection
Connecticut recently passed a bill that expands the types of entities to which billing and collection restrictions apply, placing further limitations on collection efforts by such entities and making several changes to Connecticut’s exiting laws concerning facility fees, reports the National Law Review. Among other changes, the new law prohibits hospitals, entities that are owned by or affiliated with a hospital and collection agents that receive referrals from hospitals or such other “affiliated with” or “owned by” entities from: reporting a patient to a credit rating agency for a period of one year beginning on the date that the patient first receives a bill for healthcare provided; initiating an action to foreclose a lien on a patient’s primary residence if the lien was filed to secure payment for healthcare providers; or applying to a court for an execution against a patient’s wages or otherwise seeking to garnish a patient’s wages, to collect payment for healthcare services, if such patient is eligible for the hospital bed fund.
Federal Grant Will Help Tackle Health Disparities in Connecticut
Connecticut’s Office of Health Strategy (OHS), tasked with reducing health disparities within the state, will receive $3.3 million of a $17 million grant from the Centers for Disease Control and Prevention, reports NBC Connecticut. The grant money will be spent on work by OHS and community organizations, focusing on reducing maternal and nutritional disparities, food insecurity and overcoming language and transportation barriers. Much of the grant money will go to addressing these issues in communities of color, as people of color experience significant health disparities often caused by social determinants of health.
Report: Connecticut Must Improve Health Data Collection on Race and Ethnicity
Connecticut has no statewide standards for the way its medical facilities gather, report and use patient data on race, ethnicity and language, reports the CT Mirror. Though collecting these data won’t by itself solve health disparities, a new report commissioned by the Connecticut Health Foundation explains that this step enables providers to target gaps in care experienced by people of color. The foundation stressed that collecting and analyzing such data can lead to better care and reduce inequities. While many Connecticut healthcare systems do collect some of this data, the amounts vary, and fewer organizations are using the information to address care disparities. Connecticut recently passed a bill that would require the improved collection of this data among state agencies, boards and commissions, in a way that allows for aggregation and disaggregation, as well as other mandates on data collection.
Healthcare in Connecticut is Unaffordable for Hundreds of Thousands
Approximately 18 percent (or 165,000) of households in Connecticut with adults under the age of 65 face unaffordable healthcare costs, reports CT News Junkie. These data, from a report issued by the Office of Health Strategy and the Office of the State Comptroller, show that many families in the state are spending more for healthcare than they can afford. An estimated 42 percent of households who purchase their insurance through the state’s insurance exchange face costs that exceed the affordability target, while 16 percent of households with employer-sponsored insurance experience the same burden. Officials revealed a new tool to help lower these costs, the CT Healthcare Affordability Index, which measures the impact of healthcare costs on a household’s ability to afford all basic needs.
Health Disparities and Social Determinants of Health in Connecticut
Access Health CT, Connecticut’s official health insurance marketplace, published a report summarizing findings from a data-grounded exercise designed to identify the needs and opportunities of Connecticut communities and develop recommendations to address health disparities in the state. Recommendations include reducing the cost of care and improving insurance coverage; implementing bias and cultural competency training to help providers become better attuned to implicit biases and develop skills to address them; supporting the work of Community Health Workers or Care Coordinators as “super navigators;” and centralizing data to make information more accessible/enhance reporting to better support whole person health.
Governor Unveils Plans to Reduce Cost of Healthcare, Cap Price of Prescription Drugs
Connecticut’s governor unveiled two proposals aimed at reducing the cost of healthcare, including an annual tax on insurance carriers to fund additional insurance subsidies and a plan to limit yearly increases in prescription drug costs, reports The CT Mirror. The fee on insurers would generate approximately $50 million annually to subsidize the cost of insurance for people purchasing coverage through the state’s exchange, but could also be used for other causes, including raising the Medicaid eligibility level or a reinsurance program. The Governor also proposed to limit yearly hikes in prescription drug prices to the rate of inflation plus 2 percent. Drug manufacturers exceeding that amount would be fined and revenue from the penalties would be used to subsidize health coverage.
Hospital ‘Facility Fees’ in Connecticut Reach All-Time High of $437 Million
Fees levied on insurers and patients for health services provided in hospital-owned facilities in Connecticut totaled $437.2 million last year, reaching their highest level since the state began tracking the charges in 2015, according to the Harford Business Journal. The increased revenue generated from the fees was partially driven by an 11.4 percent increase in the number of patient visits subject to a facility fee, with digestive-system and cardiovascular procedures generating more fee revenue than other service categories across the state. The average facility fee was $147 for visits billed to Medicaid, $213 for visits billed to Medicare and $426 for visits billed to commercial insurers. It is not clear what portion of the facility fees commercially insured patients ended up paying, compared to their insurer.
Survey: Most Connecticut Residents Worry About Affording Healthcare if They Get COVID-19
At the height of the coronavirus pandemic, a majority of Connecticut residents worried they would not be able to cover their medical bills if a family member were to contract COVID-19, reports the Hartford Courant. Additionally, a survey of nearly 1,000 Connecticut adults revealed that most had experienced one or more healthcare affordability burdens—such as delaying or canceling medical appointments because of high costs, opting to go without insurance entirely or struggling to pay medical bills after receiving care—in the past year. Respondents strongly supported state and federal action on healthcare affordability problems; 92 percent said the government should expand health insurance options so that everyone can afford quality coverage.
Connecticut Passes Price Caps on Insulin
The Connecticut General Assembly passed legislation that will cap the monthly cost of insulin, supplies and emergency insulin for people with insurance, according to the CT Examiner. Beginning Jan. 1, 2022, the maximum monthly out-of-pocket cost for insulin will be $25, while non-insulin medication and devices/equipment will cost $25 and $100, respectively. Additionally, anyone with diabetes will be eligible for a 30-day emergency supply of insulin at any pharmacy in the state one time per year. The law is a major win for roughly 25 percent of patients with diabetes who report rationing insulin because of cost.
Connecticut Leads States in Lawsuit Against Generic Drug Companies for Price Fixing
A coalition of 51 states and territories, led by Connecticut’s attorney general, are suing generic drug companies for price fixing, according to a press release from the attorney general’s office. The lawsuit stems from the ongoing antitrust investigation into a widespread conspiracy by generic drug manufacturers to artificially inflate and manipulate prices, reduce competition and unreasonably restrain trade for generic drugs sold across the United States.
Connecticut Governor Limits Hospital Billing to Uninsured
Connecticut's governor issued an executive order prohibiting hospitals from charging uninsured patients more than the Medicare price for their COVID-19 care, according to Modern Healthcare. The order also aligns payment for emergency and non-emergency out-of-network care by requiring insurers to pay out-of-network providers in-network prices for care during the COVID-19 public health emergency, and protects healthcare workers and facilities from lawsuits if they are “acting in good faith” to provide COVID-19 care despite shortages or capacity issues.
Governor Signs Executive Orders Reducing Healthcare Costs for Connecticut Residents
Connecticut’s Governor signed two executive orders to directly address healthcare costs, primary care spending and quality of care for individuals, businesses and the state government, according to Robert Wood Johnson’s State Network. The orders direct the Office of Health Strategy to establish statewide healthcare cost growth and quality benchmarks in addition to a primary care spending target, and direct the Department of Social Services to improve public transparency of Medicaid costs and quality.
Racial Disparities Persist in CT Healthcare, Two Groups Find
While Connecticut has led national efforts in public insurance reform, research shows that significant health disparities persist between the state’s residents of color and white residents, reports the CT Mirror. Specifically, Black and Latino residents are more likely than white residents to be uninsured, to die before reaching adulthood and to report being in poor health. Latino adults, in particular, were more than twice as likely as white residents to say they went without seeing a doctor in the past 12 months because of the cost.
Healthcare Affordability Standard Tool to Influence Policy Debates
Connecticut’s state comptroller and Office of Health Strategy are developing a “healthcare affordability standard” to calculate how much money individuals and families in the state must earn in order to afford healthcare without compromising other basic needs, like food and housing, reports Hartford Business. According to officials, understanding the threshold at which healthcare becomes unaffordable is vital to creating sound policies. The tool is anticipated to launch in Spring of 2020.
Researcher IDs Connecticut’s Most Litigious Hospital; Thousands of Patients Sued Annually
One Connecticut hospital stands alone when it comes to pursuing patients in small claims court over unpaid medical bills, according to Hartford Business. Research from the UConn Health Disparities Institute revealed that Danbury Hospital filed nearly half of the 13,824 total medical debt cases in Connecticut in 2016. The hospital claimed $8.8 million in debt from these lawsuits, compared to $10.4 million claimed in lawsuits filed by all other Connecticut hospitals that sued patients for medical debt that year. The finding has prompted Danbury Hospital to review its debt-collection policies.
CT Moves Closer to Healthcare 'Excellence' Referral Network
Connecticut’s “Centers of Excellence” network will enable state residents to identify which providers perform best for certain procedures, helping them make informed decisions about where to receive their care, reports The CT Mirror. By steering patients to providers who offer cost-effective treatments, the state hopes to reduce its healthcare costs by millions of dollars in the 2019 and 2020 fiscal years combined. The resource will be released in 2020 and will serve an estimated 210,000 state employees, retirees and dependents.
Connecticut Man Got Price Estimates Before Surgery — And a Bill That Was 50% More
A Connecticut man received a bill for double the amount he was quoted for a hernia repair after contacting his hospital, surgeon and anesthesiologist prior to the procedure to determine the expense, according to Kaiser Health News. Unlike prices quoted in other industries, hospital estimates are often inaccurate and there is no legal obligation that they be correct, or even issued in good faith. After an emotionally draining process of dealing with billing departments and following up with his insurer, the bill was eventually written off. However, many other patients aren’t as proactive and wouldn’t fight a bill they could afford to pay.
Connecticut Holds Hospitals Accountable for Meaningful Community Benefit Investment
Connecticut is using certificate of need (CON) regulations to hold hospitals accountable for making meaningful investments in their communities’ health, according to the National Academy for State Health Policy. In a recent CON agreement, the Connecticut Office of Health Strategy mandated that merging hospitals: adopt evidence-based interventions to address community needs; explain how patient outcomes will be measured and reported to the community; and increase the total dollars spent on community benefit activities by at least one percent each year for the next five years. These activities must directly address the health and health-related social needs identified by the hospital’s Community Health Needs Assessment. While the CON conditions are time-limited, they demonstrate what is possible when states use their policy levers to maximize community benefits investments.
Office of Health Strategy Launches Online Healthcare Rating System
Connecticut’s Office of Health Strategy launched a free, online tool intended to help consumers, businesses and healthcare providers navigate the state’s vast system of care, reports The CT Mirror. The website’s two key elements–a quality scorecard and a cost estimator–will allow users to compare the quality and cost of medical care at 19 of the state’s healthcare organizations. Organizations are also evaluated on patient experience in four categories: office staff, provider communication, timely care and overall patient experience. In addition, users can compare the overall performance rating of provider networks across all quality measures. Connecticut is one of the first states to create a rating system that evaluates the performance of provider networks rather than individual providers.
New CT Hospital Cost Caps Could Chip Away at Rising Healthcare Spending
State regulators approved two major hospital mergers and acquisitions under the condition that the organizations agreed to healthcare cost price caps tied to the Consumer Price Index, reports the Hartford Business Journal. This type of agreement is a first for Connecticut and one of the most stringent cost controls ever placed on hospital combinations in the state. Compared to states like Massachusetts and Rhode Island, Connecticut’s caps are relatively modest. Nevertheless, they are an important protection against rising healthcare costs, which have historically increased with consolidation
Understanding Community Health Workers: Who they are and why they matter for Connecticut
Community health workers have the potential to help improve health outcomes, reduce costs and reduce health disparities. Despite this, the role of community health workers in the healthcare system remains precarious and not widely understood. A report released by the Connecticut Health Foundation aims to shed light on the work community health workers are doing in Connecticut and their potential to bridge gaps between clinical care and patients’ lives. This report complements previous research published by the Connecticut Health Foundation, including a brief and report identifying specific ways community health worker services can produce a positive return on investment and a report detailing how 15 other states handle certification for community health workers.
Reduced Cost of Specialty Care Using Electronic Consultations for Medicaid Patients
Specialty care accounts for a significant and growing portion of year-over-year Medicaid cost increases. Some referrals to specialists may be avoided and managed more efficiently by using electronic consultations. A study in Health Affairs found that linking primary care providers with specialists in dermatology, endocrinology, gastroenterology and orthopedics in Connecticut using an electronic platform reduced the need for face-to-face visits, saving an average of $82 per patient per month. Researchers concluded that expanding the use of electronic consultations for Medicaid patients and reimbursing the service could result in substantial savings while improving access to and timeliness of specialty care and strengthening primary care.
Conn. Lawmakers, Governor Wrangle Over Telemedicine
Connecticut’s U.S. congressional delegation is at odds with the governor over the failure to apply for an expansion of the HUSKY program that would give low-income residents access to new telemedicine services, especially for psychiatric care and substance abuse treatment, reports The CT Mirror. Five Democrats representing Connecticut in the U.S. House of Representatives are pressing the Malloy administration to apply for the waiver, which would allow the state’s doctors and hospitals to receive Medicaid reimbursements for their services when they treat HUSKY patients through telemedicine. The Malloy administration says the process for obtaining permission to add these services is lengthy, may not achieve the desired results and is not currently a priority. Connecticut is the only state in the nation that has not requested a waiver from the Department of Health and Human Services to incorporate telemedicine into its Medicaid program.
In a State of Great Wealth, All the Health Care Some Can Afford
Tens of thousands of Connecticut residents lack access to adequate healthcare, despite the state’s tremendous wealth and strong embrace of the federal Affordable Care Act, according to The Connecticut Mirror. While Connecticut once had a generous social safety net that elevated its poorest residents above their counterparts in most other states, it has since been eroded by massive budget deficits, which could get worse in the near future. Advocates worry that changes on the horizon could mean greater barriers to healthcare for many Connecticut residents – low-income individuals and families, those who rely on safety-net clinics for care, middle-class earners whose income has been squeezed by healthcare costs, and those with insurance plans that increasingly require them to pay more for care.
Survey: CT Residents Burdened by Healthcare Costs, Complexity; Want Reforms
A survey conducted Altarum’s Healthcare Value Hub for the Universal Health Care Foundation of Connecticut revealed that residents across the political spectrum want state laws that require healthcare pricing transparency and make it easier to navigate the complex system, reports Hartfordbusiness.com. The survey found that half of survey respondents had experienced healthcare affordability burdens in the previous 12 months. Of that group, four in five said they had delayed or skipped a doctor visit, medical procedure or test, cut pills in half or skipped doses, or had trouble accessing mental healthcare due to cost. Though lower-income households had the highest reported affordability burdens, 42 percent of households making more than the state's median income reported experiencing cost burdens. Respondents supported a number of steps to remedy affordability problems, such as showing patients a "fair cost" for specific procedures, requiring medical providers and insurers to give up-front cost estimates and giving the state Attorney General the authority to prevent price gouging on prescription drugs.
Feds OK First Stage of New Connecticut Hospital Taxing System
The U.S. Centers for Medicare and Medicaid Services approved a significant increase in Connecticut's annual tax on hospitals—from roughly $556 million to $900 million, reports The CT Mirror. The state will redistribute much of the revenue back to its hospital industry through increased hospital payments, but the new taxing arrangement will allow Connecticut to draw an additional $150 million in federal money annually through its Medicaid program. This back-and-forth arrangement is currently employed by a number of states.
Connecticut Passes Drug Transparency Law
Connecticut is one of several states that have recently enacted drug cost transparency laws, designed to make drug pricing information accessible so states can eventually take action on price gouging, reports NASHP. The new Connecticut law requires drug makers, health insurers, and pharmacy benefit managers (PBM) to disclose a wide assortment of information on price increases. Drug makers must justify large increases, insurers must report them when filing rate requests and PBMs must report how much they collect in rebates and how much they keep.
Drug-Price Transparency Bill Passes CT Legislature with No Dissent
A new Connecticut law requires drug companies, health insurers and pharmacy benefit managers to disclose a wide range of drug pricing information to the state, reports CT Mirror. Key provisions that go into effect on Jan. 1, 2020, include: requiring drug companies to justify potentially unwarranted drug price increases over specified periods of time; requiring insurers to identify the 25 drugs with the highest cost to the plan, the 25 with the greatest year-over-year price increases and the 25 most frequently prescribed, as well as the premium growth that is attributable to prescription drugs; and requiring PBMs to report how much they collect in rebates and the share that they keep. Insurers will also be required to report whether they use the rebates to offset premiums or pass the money down to residents at the pharmacy counter. The bill does not include a previous requirement that the majority of rebates from drug companies be passed down to consumers when they buy drugs at pharmacies.
Healthcare by the Numbers: Gathering Data on Racial Disparities
Connecticut Voices for Children is partnering with Health Equity Solutions to propose legislation that would standardize guidelines across state agencies for collecting data related to race and ethnicity in healthcare outcomes, reports WNPR. The bill would provide better training for the healthcare professionals who collect the data and make the data easily shareable, in addition to increasing the specificity of the data collected so that outcomes for smaller ethnic groups can be more easily tracked. Advocates assert that increasing the availability of data on smaller racial and ethnic minorities will increase social justice, save money on costly disease management and get more of the state's population healthy and contributing to the economy.
Connecticut Establishes Office of Health Strategy
Connecticut has launched a new Office of Health Strategy, designed to implement comprehensive, data-driven strategies that promote equal access to high-quality healthcare, control costs and ensure better health for state residents. The office will bring together the formerly independent State Innovation Model (SIM) Project Management Office, Health Information Technology Office, Office of Health Care Access and All Payers Claims Database to combine critical data sets and health information exchange efforts and allow for collaboration with many stakeholders, including state agency partners. “Connecticut has made strong progress on healthcare coverage and accessibility, but there is much more we need to do to address health outcomes, healthcare costs, health inequities and care delivery and payment reforms. Healthcare isn’t a partisan issue, the Office of Health Strategy will help us move forward collaboratively to address these issues with our stakeholders,” said Executive Director Vicki Veltri.
Governor Proposes State Office of Health Strategy
In November, Connecticut passed legislation to establish an Office of Health Strategy, which will oversee all of the state’s major health reform and planning initiatives. These include the Health Information Technology Office, the State Innovation Model Management Office, the All-Payer Claims Database and the Office of Healthcare Access. “The Office of Health Strategy is an opportunity to ensure better health outcomes, to lower costs and to create a more efficient healthcare system,” said Lt. Gov. Nancy Wyman. “This signifies important progress that must continue—and is most effectively coordinated by a single entity.”
Piercing the Darkness in Connecticut: A Supplement to the National Price Transparency and Physician Quality Report Card
For the past several years, healthcare costs in Connecticut have continued to rise, despite evidence suggesting that consumers are not uniformly receiving high quality care. Additionally, the state received double F’s on the Leapfrog Group’s Price Transparency and Physician Quality Report Card for its ability to help consumers find the information they want and need to compare the price and quality of their healthcare. A recent report released by Altarum examines Connecticut’s cost and quality issues, highlighting the inefficient management of hospital expenses and arguing against the continued inflation of prices irrespective of healthcare value.
Connecticut Governor Signs Consumer-Protection Drug Law
A new Connecticut law will outlaw “gag clauses” in pharmacy benefit-manager contracts that now bar pharmacists from telling consumers when they could save money by paying out of pocket for generic drugs that can cost less than the co-pay for a covered brand-name drug, according to the Connecticut Mirror. The bill also would require insurers to give better notice to consumers regarding the cost of using out-of-network labs.
Measuring Health Insurance Literacy in Connecticut
Many Connecticut residents struggle to understand insurance terminology and perform the financial calculations required in today’s complex insurance plan designs, according to UCONN Health. These problems are difficult to overcome, but a state-wide strategy aimed ultimately at enhancing the value of health insurance for all is needed.
SNOMED CT Code Framework Will Aid EHR Reporting, Interoperability
A coalition of pharmacy societies has released a new framework for mapping medication therapy management services to the SNOMED CT codes used for EHR documentation, interoperability efforts, and quality reporting. Unlike ICD-10, which is primarily geared toward recording diagnoses and procedures, SNOMED CT attempts to capture a more holistic view of the patient and his or her experiences, including socioeconomic data, medication use, lifestyle behaviors and family history.
Starling Physicians Partners with Aetna on Oncology Medical Home Model
Starling Physicians will partner with Aetna to participate in an oncology medical home model designed to improve patient experience by enhancing delivery of quality and value in cancer care. The model will be centered around the whole person, with evidence-based, integrated and personalized medical care, with a focus on quality and safety; and enhanced access to care.
Connecticut’s FAIR Health App Aims to Improve Price Transparency, Health Insurance Literacy
A new free mobile application, "FH Cost Lookup CT," enables both insured and uninsured consumers to estimate the region-specific costs of medical and dental procedures, reports Healthcare Finance. The app was launched by FAIR Health and funded by a grant from the Connecticut Health Foundation. The application is available in both English and Spanish, includes region-specific costs in neighboring states of New York, Massachusetts and Rhode Island, and provides educational articles to explain the fundamentals of health coverage. It is driven by healthcare prices from FAIR Health’s database of more than 21 billion claims for privately billed medical and dental procedures since 2002.
Connecticut Health Policy Project Releases "Basics of Health Policy" Manual
The Connecticut Health Policy Project released a report and training module aimed toward students, interns, and volunteers that discusses the basics of health policy. The report gives an overview of public insurance, private insurance, the uninsured, healthcare financing, healthcare reform, and the role of states.
Sweeping Plan Put Forward To Control Rising Healthcare Costs
A state-hired consulting firm presented a plan to Connecticut’s Health Care Cabinet that called for the largest reorganization and consolidation of health-related state agencies in two decades, according to The Connecticut Mirror. The proposal urged the creation of the Connecticut Health Authority, which would absorb the responsibilities of more than six state agencies and would create a quasi-independent oversight agency, the Office of Health Reform. The Office of Health Reform would track and limit healthcare cost increases. The proposal also called for the creation of “consumer care organizations” -- networks of healthcare providers that would receive large payments based on the total number of consumers using the services in its network. Providers in consumer care organizations would be paid based on the quality of their care.
Consumers Must Have a Voice in Healthcare Mergers
Many Connecticut residents still don’t know that by the end of this year, Anthem Insurance Co. and Cigna may merge, forcing us all into a dire situation, according to Frances Padilla of the Universal Health Care Foundation of Connecticut. Mergers are justified on the basis of increased efficiency and opportunity for innovation, but past experience doesn’t uphold those claims. They should be carefully questioned, because they can be expected to increase health insurance premiums, and cause deductibles, co-pays, and co-insurance out-of-pocket costs to spike.
Connecticut Law Addresses Surprise Facility Fee Charges
A new law in Connecticut, which goes into effect January 1, 2016, requires hospitals and health systems that acquire a physician practice to notify all patients within 30 days after the acquisition that their outpatient services will now include facility fees, reports Modern Healthcare. Additionally, hospital bills must clearly state that the fee is to be used for the hospital's operational expenses, that the patient would likely be charged less at an outpatient care center not owned by a hospital and that the patient has a right to request a reduction in the facility fee. The provisions are part of a larger bill passed in June aimed at improving price transparency for patients.
Addressing State Healthcare Challenges Through Regulation: Use of a Public Utility Model
Drawing on examples from several states, this report explores the pros and cons of a public utility model for healthcare for Connecticut.
Medicare Advantage Plans Need Tougher Oversight, GAO Says
Connecticut Health I-Team: Federal investigators have found that Medicare officials rarely enforce rules for private insurance plans intended to make sure beneficiaries will be able to see a doctor when they need care. It's a problem many Connecticut seniors know too well. In 2013, UnitedHealthcare, the nation's largest health insurance company, dropped hundreds of healthcare providers from its Connecticut Medicare Advantage plan, including 1,200 doctors at the Yale Medical Group and Yale-New Haven Hospital. Medicare Advantage beneficiaries scrambled to find new insurance or new doctors while the Fairfield and Hartford counties medical associations went to court to try to stop the terminations.
Obamacare and Hospital Finances, in Nine Charts
The Connecticut Mirror: The financial condition of Connecticut’s hospitals, and how they’ve fared under the federal health law, has been a source of dispute among state lawmakers. Hospitals have faced repeated funding cuts and increased taxes in recent state budgets. This article looks at recently released financial data from the 2014 fiscal year, the first after the major coverage expansion provisions of the health law took effect.
State Trims Most Insurers' Proposed Rate Hikes
Hartford Courant: Most insurance companies selling health plans in the state's individual market will get to raise customers' premiums in 2016, but not by as much as they proposed, and ConnectiCare Benefits—the largest carrier in the state's insurance exchange—will have to lower rates, according to decisions released by the Connecticut Insurance Department.
Prevention and Public Health Fund at Work in Connecticut
This report by the Trust for America’s Health, financed by the Prevention and Public Health Fund, details public health and prevention activities around the state.
Connecticut Health Care Costs
The Connecticut Health Policy Project released a report that examines how much Connecticut spends on healthcare. The report discusses Connecticut health spending and projected growth rates. The report also covers who pays the healthcare costs, where each healthcare dollar is spent, and what factors are driving healthcare costs, both nationally and in Connecticut.
The Power of Data: Consumer Involvement and Accountability for Connecticut’s All-Payer Claims Database (APCD)
This report, funded by the Connecticut Health Foundation, identifies opportunities to influence the design, development and governance of Connecticut’s APCD to maximize its usefulness specific to patient safety and health equity/disparities researchers, and consumers. Key findings include: (1) APCDs are providing consumers access to patient safety and quality reports to make informed healthcare decisions, (2) health equity/disparities researchers are working together in data, cost, and quality collaboratives, (3) NIH is funding health data research using the APCD, (4) state cost and quality councils are utilizing APCD data to regulate hospital performance and reimbursement, (5) APCDs are predominantly operating within state agencies, independent of health insurance exchanges, and (6) opportunities for engaging stakeholders to influence the design and implementation of Connecticut’s APCD.
VBID in Action: A Profile of Connecticut's Health Enhancement Program
This report evaluates the early implementation of Connecticut's Health Enhancement Program, a new value-based insurance design plan for state workers created in partnership between the governor's office, a coalition of unions representing state employees.