Maryland Residents Struggle to Afford High Healthcare Costs; Worry about Affording Healthcare in the Future; Support Government Action across Party Lines
Key Findings
A survey of more than 1,300 Maryland adults, conducted from July 6 to July 20, 2022, found that:
- Nearly 3 in 5 (55%) experienced at least one healthcare affordability burden in the past year;
- More than 4 in 5 (82%) reported worry about affording healthcare in the future;
- Lower-income respondents and respondents with disabilities were more likely to report go without care and incurring debt due to healthcare costs; and
- Across party lines, respondents expressed strong support for government-led solutions.
A Range of Healthcare Affordability Burdens
Like many Americans, Maryland adults experience hardship due to high healthcare costs. All told, more than half (55%) of respondents reported experiencing one or more of the following healthcare affordability burdens in the prior 12 months:
1) Being Uninsured Due to High Costs
More than one-third (36%) of uninsured respondents cited “too expensive” as the major reason for not having coverage, far exceeding other reasons like “don’t need it” and “don’t know how to get it.”
2) Delaying or Going Without Healthcare Due to Cost
Nearly half (48%) of all respondents reported delaying or going without healthcare during the prior 12 months due to cost:
- 30%—Skipped needed dental care
- 26%—Delayed going to the doctor or having a procedure done
- 23%—Cut pills in half, skipped doses of medicine or did not fill a prescription1
- 21%—Avoided going to the doctor or having a procedure done altogether
- 21%—Skipped a recommended medical test or treatment
- 17%—Had problems getting mental healthcare or addiction treatment
- 10%—Skipped or delayed getting a medical assistive device
Moreover, cost and the ability to get an appointment were the most frequently cited reasons for not getting needed medical care (each reported by 20% of respondents), exceeding a host of other barriers, such as difficulty finding transportation or a lack of childcare.
3) Struggling to Pay Medical Bills
Other times, respondents got the care they needed but struggled to pay the resulting bill. One out of three (32%) experienced one or more of these struggles to pay their medical bills:
- 12%—Used up all or most of their savings
- 11%—Were contacted by a collection agency
- 10%—Racked up large amounts of credit card debt
- 8%—Were unable to pay for basic necessities like food, heat or housing
- 7%—Borrowed money, got a loan or another mortgage on their home
- 6%—Were placed on a long-term payment plan
Of the various types of medical bills, the ones most frequently associated with an affordability barrier were dental bills, doctor bills and prescription drugs. The high prevalence of affordability burdens for these services likely reflects the frequency with which Maryland respondents seek these services. Trouble paying for dental bills likely reflects lower rates of coverage for these services.
High Levels of Worry About Affording Healthcare in the Future
Maryland respondents also exhibit high levels of worry about affording healthcare in the future. Four in five (82%) reported being “worried” or “very worried” about affording some aspect of healthcare in the future, including:
- 66%—Cost of nursing home or home care services
- 62%—Medical costs when elderly
- 61%—Health insurance will become unaffordable
- 57%—Medical costs in the event of a serious illness or accident
- 53%—Cost of dental care
- 49%—Prescription drugs will become unaffordable
- 35%—Cost of treatment for coronavirus/COVID-19
While two of the most common worries—affording the cost of nursing home or home care services and medical costs when elderly—are applicable predominantly to an older population, they were most frequently reported by respondents ages 35-44. This suggests that Maryland respondents may be worried about affording the cost of care for both aging parents and themselves.
Worry about affording healthcare was highest among respondents living in lower-income households, those with Maryland Medicaid healthcare coverage, respondents of color and those living in households with a person with a disability (see Table 1). More than 4 in 5 (89%) of respondents with household incomes of less than $50,000 per year2 reported worrying about affording some aspect of coverage or care in the past year. Still, the vast majority of Maryland respondents of all incomes, insurance types, races, ethnicities and levels of ability statewide are somewhat or very concerned about affording some aspect of coverage or care.
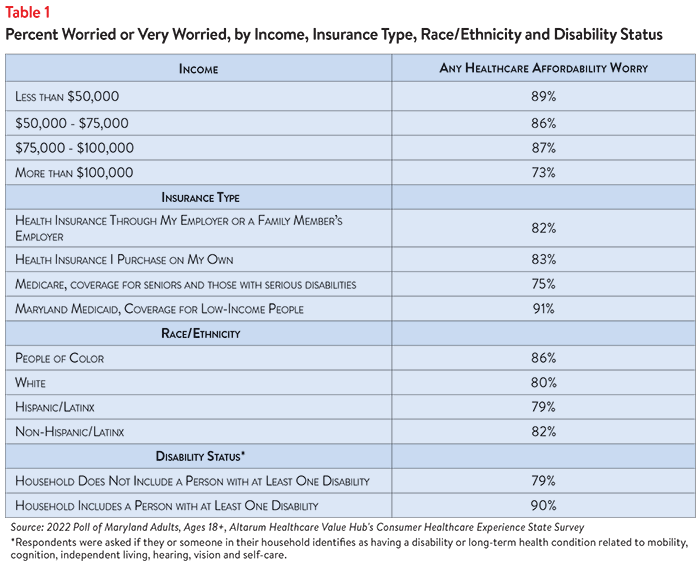
Concern that health insurance will become unaffordable is also more prevalent among certain groups of Maryland adults. By insurance type, respondents with coverage they purchase on their own most frequently reported worrying about affording coverage, followed by those with Maryland Medicaid (see Figure 1).
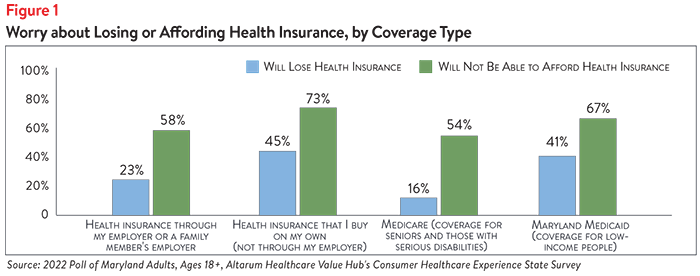
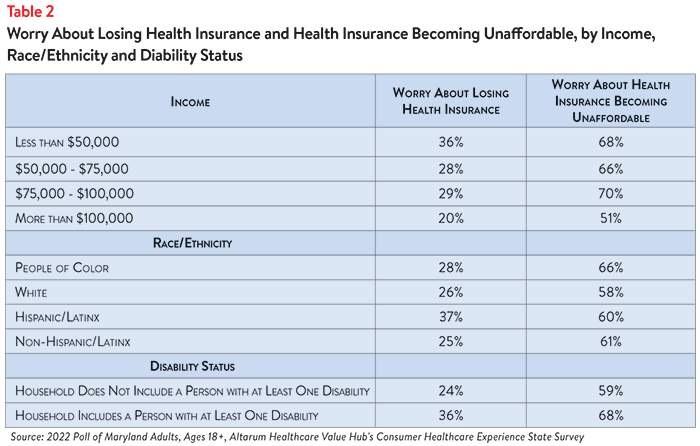
Those with household incomes between $75,000 and $100,000 reported the highest rates of worry about affording health insurance coverage, though individuals in lower income brackets reported only slightly lower levels of worry. Those living in households with a person with a disability were more likely to report being concerned about affording health insurance than their non-disabled counterparts. Respondents of color also reported higher rates of worry about affording health insurance coverage than their white counterparts (see Table 2).
Concerns about affording coverage exceeded fears about losing coverage across all income groups, disability statuses and coverage types.
Differences in Healthcare Affordability Burdens
The survey also revealed differences in how Maryland respondents experience healthcare affordability burdens by income, age, insurance type, race and disability status.
Income and Age
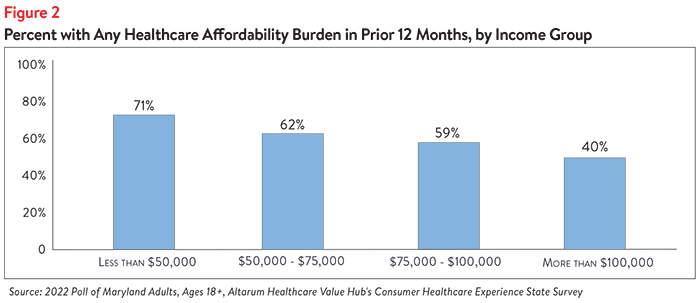
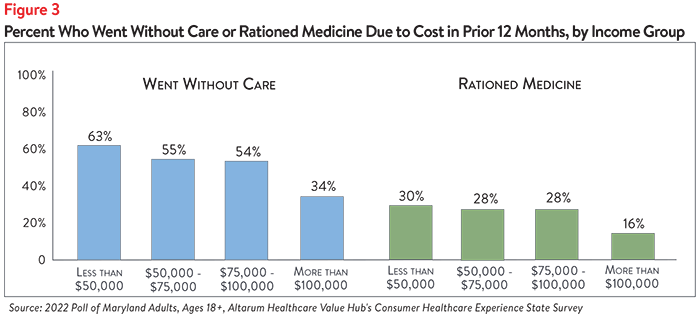
Unsurprisingly, respondents at the lowest end of the income spectrum most frequently reported experiencing one or more healthcare affordability burdens, with nearly 3 out of 4 respondents (71%) earning less than $50,000 reporting struggling to afford some aspect of coverage or care in the past 12 months (see Figure 2). This may be due, in part, to respondents in this income group reporting high rates of going without care and rationing their medication due to cost (see Figure 3).
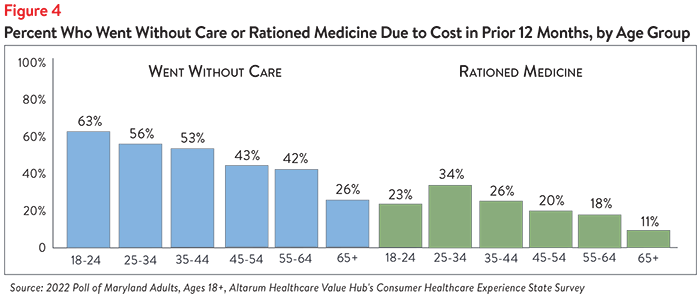
Further analysis revealed that Maryland respondents ages 18-44 are more likely to report going without care due to cost than respondents ages 45 and older (see Figure 4). Respondents ages 25-34 most frequently reported rationing medication due to cost, compared to other groups.
Insurance Type
Maryland Medicaid respondents reported the highest rates of going without care due to cost, while rationing medication was reported most by both respondents that buy their own healthcare coverage and those who receive Medicaid (see Table 3). Still, nearly half of respondents with employer-sponsored insurance reported going without care due to cost.
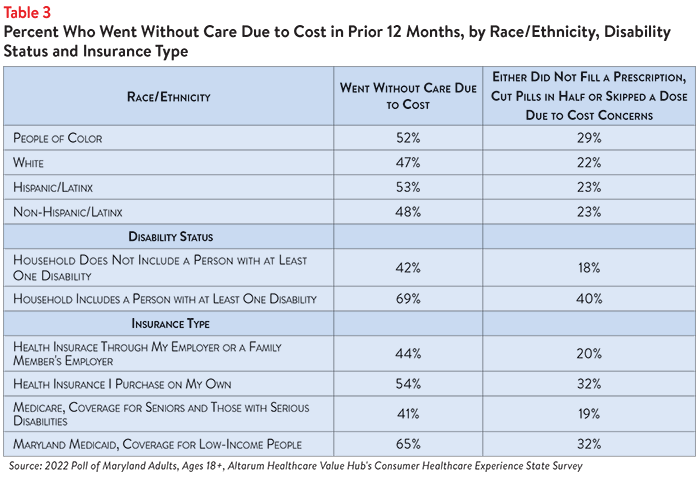
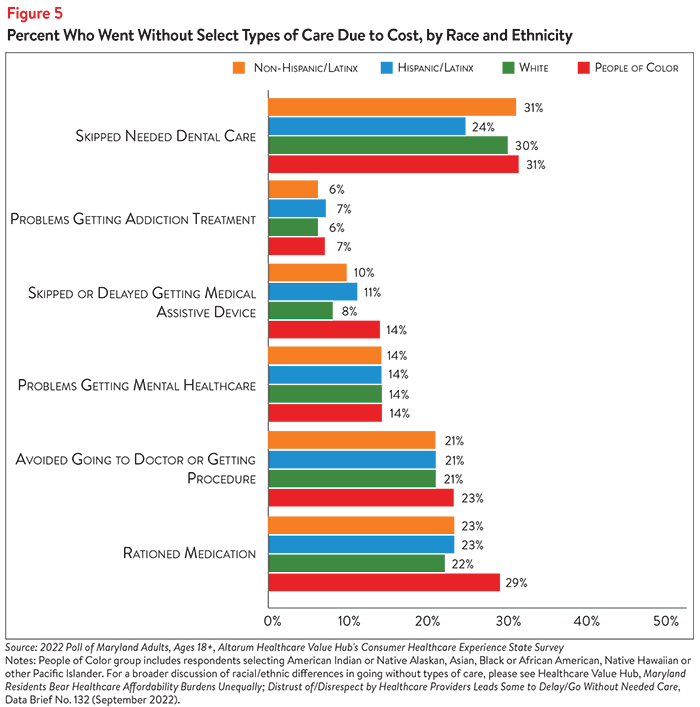
Race
Respondents of color reported higher rates of going without care and rationing medication due to cost when compared to white respondents (see Table 3). Further analysis showed that respondents of color had slightly higher rates of reporting problems getting addiction treatment and of skipping or delaying getting a medical assistive device (see Figure 5).
Disability Status
Of all the demographic groups measured, respondents living in households with a person with a disability reported the highest rates of going without care and rationing medication due to cost in the past 12 months. Nearly 7 in 10 (69%) of respondents in this group reported going without some form of care and well over one-third (40%) reported rationing medication, compared to 42% and 18% of respondents living in households without a person with a disability, respectively (see Table 3). Respondents living in households with a person with a disability also more frequently reported delaying or skipping getting mental healthcare, addiction treatment and dental care due to cost concerns, among other healthcare services, than those in households without a person with a disability (see Table 4).
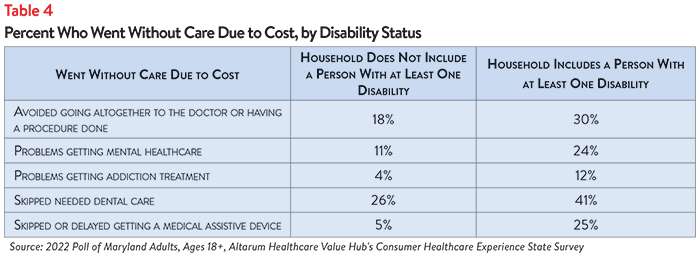
Those with disabilities also face healthcare affordability burdens unique to their disabilities—25% of respondents reporting a disability in their household delayed getting a medical assistive device such as a wheelchair, cane/walker, hearing aid or prosthetic limb due to cost. Just 5% of respondents without a person with a disability (who may have needed such tools temporarily or may not identify as having a disability) reported having this experience.
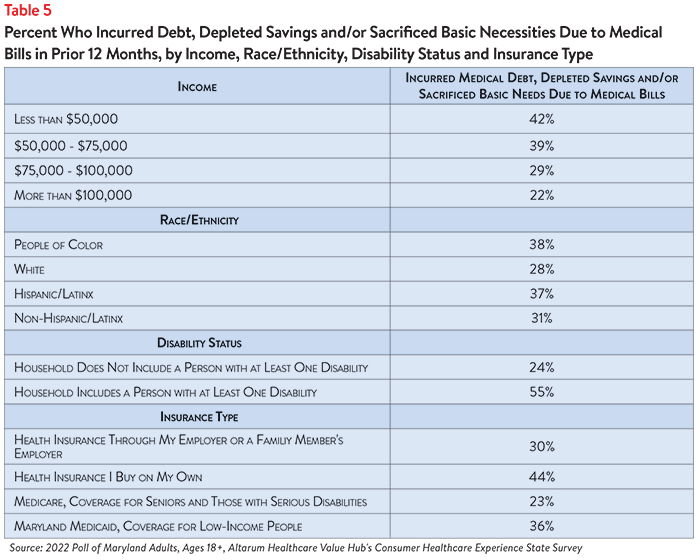
Encountering Medical Debt
The survey also showed differences in the prevalence of financial burdens due to medical bills, including going into medical debt, depleting savings and being unable to pay for basic necessities (like food, heat and housing) by income, race, ethnicity, disability status and insurance type. Thirty-eight percent of respondents of color reported going into debt, depleting savings or going without other needs due to medical bills, compared to 28% of white respondents (see Table 5). An even greater disparity was seen for respondents with a household member with a disability, with more than half (55%) reporting going into debt or going without other needs due to medical bills, compared to 24% of respondents living in households without a disabled member. In addition, respondents who purchase health insurance on their own reported the highest rate of the above financial burdens due to medical bills (44%) compared to all other insurance types.
Healthcare affordability burdens often occur alongside systemic mistreatment in the health system, making it even more difficult for marginalized communities to access care. For further details, see the brief: Maryland Residents Bear Healthcare Affordability Burdens Unequally; Distrust of/Disrespect by Healthcare Providers Lead Some to Delay/Go Without Needed Care, Data Brief No. 132 (October 2022).
Dissatisfaction with the Health System and Support for Change
In light of Maryland respondents’ healthcare affordability burdens and concerns, it is not surprising that they are dissatisfied with the health system:
- Just 33% agreed or strongly agreed that “we have a great healthcare system in the U.S.,”
- While 72% agreed or strongly agreed that “the system needs to change.”
To investigate further, the survey asked about both personal and governmental actions to address health system problems.
Personal Actions
Maryland respondents see a role for themselves in addressing healthcare affordability. When asked about specific actions they could take:
- 50% of respondents reported researching the cost of a drug beforehand, and
- 74% said they would be willing to switch from a brand name to an equivalent generic drug if given the chance.
When asked to select the top three personal actions they felt would be most effective in addressing healthcare affordability (out of ten options), the most common responses were:
- 68%—Take better care of my personal health
- 37%—Research treatments myself, before going to the doctor
- 32%—Do more to compare doctors on cost and quality before getting services
- 27%— Write or call my STATE representative asking them to take action
- 23%—Write or call my FEDERAL representative asking them to take action
However, 22% of respondents chose the response “There is not anything I can do personally to make our health system better,” as one of their top three personal actions.
Government Actions
But far and away, Maryland respondents see government as the key stakeholder that needs to act to address health system problems. Moreover, addressing healthcare problems is one of the top priorities that respondents want their elected officials to work on.
At the beginning of the survey, respondents were asked what issues the government should address in the upcoming year. The top vote getters were:
- 49%—Economy/Joblessness
- 44%—Healthcare
- 32%—Taxes
When asked about the top three healthcare priorities the government should work on, the top vote getters were:
- 52%—Address high healthcare costs, including prescription drugs
- 37%—Preserve consumer protections preventing people from being denied coverage or charged more for having a pre-existing medical condition
- 32%—Improve Medicare, coverage for seniors and those with serious disabilities
- 32%—Get health insurance to those who cannot afford coverage3
Of more than 20 options, Maryland respondents believe the reason for high healthcare costs is unfair prices charged by powerful industry stakeholders:
- 74%—Drug companies charging too much money
- 71%—Insurance companies charging too much money
- 70%—Hospitals charging too much money
When it comes to tackling costs, respondents endorsed a number of strategies, including:
- 92%—Require insurers to provide up-front cost estimates to consumers
- 91%—Make it easy to switch insurers if a health plan drops your doctor
- 91%— Show what a fair price would be for specific procedures
- 90%—Require hospitals and doctors to provide up-front cost estimates to consumers
- 90%—Require drug companies to provide advanced notice of prices increases and information to justify those increases
- 90%—Authorize the Attorney General to take legal action to prevent price gouging or unfair prescription drug price hikes
- 90% —Ensure patients can’t be charged out-of-network prices if they encounter an out-of-network provider through no fault of their own
Support for Action Across Party Lines
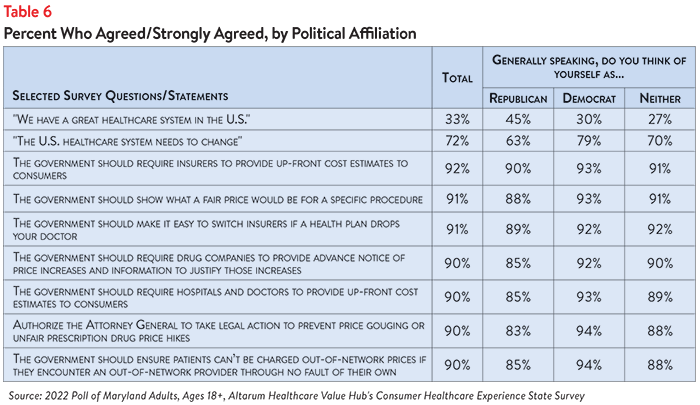
There is also remarkable support for change regardless of respondents’ political affiliation (see Table 6).
The high burden of healthcare affordability, along with high levels of support for change, suggest that elected leaders and other stakeholders need to make addressing this consumer burden a top priority. Moreover, the COVID crisis has led state residents to take a hard look at how well health and public health systems are working for them, with strong support for a wide variety of actions. Annual surveys can help assess whether or not progress is being made.
Notes
1. Of the current 48% of Maryland respondents who encountered one or more cost-related barriers to getting healthcare during the prior 12 months, 17% did not fill a prescription, while 15% cut pills in half or skipped doses of medicine due to cost.
2. Median household income in Maryland was $87,063 (2016-2020). U.S. Census, Quick Facts. Retrieved from: U.S. Census Bureau QuickFacts: Maryland
3. Two in three (67%) of respondents said that they would consider using their tax forms to sign up for health insurance if they or their family needed it. This high level of interest persisted across racial, ethnic and income groups, with the highest levels of interest among Hispanic/Latinx respondents (65%) and those earning between $75,000 and $100,000 (72%).
Methodology
Altarum’s Consumer Healthcare Experience State Survey (CHESS) is designed to elicit respondents’ unbiased views on a wide range of health system issues, including confidence using the health system, financial burden and views on fixes that might be needed.
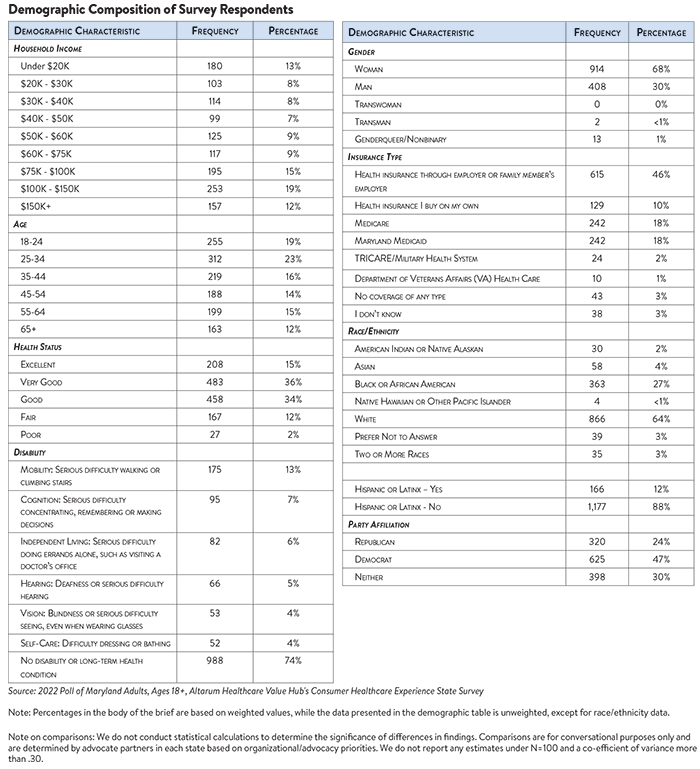
The survey used a web panel from Dynata with a demographically balanced sample of approximately 1497 respondents who live in Maryland. The survey was conducted in English or Spanish and restricted to adults ages 18 and older. Respondents who finished the survey in less than half the median time were excluded from the final sample, leaving 1,343 cases for analysis. After those exclusions, the demographic composition of respondents was as follows, although not all demographic information has complete response rates: