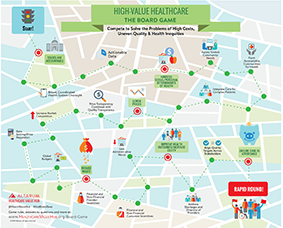
Solving the Healthcare Value Puzzle: The Board Game
Move over SimCity, Dungeons & Dragons and Monopoly – there’s a new game in town.
Attendees of the Hub’s in-person conference know that we take great pride in our opening night healthcare value-themed gameshow that gets everyone “warmed up” for the substantive discussions ahead. Because 2019’s meeting was virtual, we decided to continue our tradition with the first-ever, health policy board game.
Below, we included fun questions from our board game so you can play too! Click on the questions to revesl the answer and a link to additional resources. Share your experience with us by tagging @HealthValueHub on Twitter and using the hashtag #HubBoardGame.
Question 1:
Approximately how many healthcare quality measures are in use today: 100, 500, 750 or more than 1,000?
Answer:
More than 1,000. The National Quality Forum (NQF) has endorsed over 700 measures, but the federal government and other payers also use measures not endorsed by the NQF. In 2015, the Wall Street Journal reported that 33 federal programs asked providers to submit data on 1,675 quality measures.
Learn more: https://www.wsj.com/articles/debate-heightens-over-measuring-health-care-quality-1422661664
Answer:
Wyoming
Learn more: http://chirblog.org/will-it-fly-wy-end-run-air-ambulance/
Answer:
TRUE: The Institute of Medicine estimated that over half of treatments delivered did not have clear evidence of effectiveness as of 2009.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/comparative-effectiveness-research
Question 4:
Which is the ONLY state that pays hospitals using an ALL PAYER, global budget system?
Answer:
Maryland is unique for its method of paying hospitals and the results are promising.
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/hospital-rate-setting-promising-challenging-replicate
Answer:
TRUE
Learn more: https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-august-2019/
Answer:
Sin Taxes
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/sin-taxes
Answer:
80% or more of collected premiums must be spent on medical care.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/medical-loss-ratio
Question 8:
TRUE or FALSE: Patient Shared Decision-making improves quality of care.
Answer:
TRUE: Patient shared decision-making increases responsiveness to patients’ goals and needs, and increases compliance with a treatment plan.
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/consumer-benefits-patient-shared-decision-making/
Answer:
Mixed, reflecting, in part, the diversity of states’ approaches.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/certificate-need
Question 10:
Which state was the first in the nation to cap the price of insulin?
Answer:
Colorado
Learn more: https://www.usatoday.com/story/news/nation/2019/05/25/colorado-first-state-cap-co-pays-insulin/1235794001/
Question 11:
TRUE or FALSE: Aging of the population is an important driver of growth in health spending per person.
Answer:
FALSE: Aging has little impact in year-over-year growth in per person spending.
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/aging-population1
Question 12:
In 2019, which state began a demonstration project that implements global budgets for rural hospitals?
Answer:
Pennsylvania. Unlike the Maryland model, the global budgets are not the same across all payers.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/global-budgets
Answer:
Emergency services
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/community-health-needs-assessment
Answer:
Nearly 50%
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/provider-directory-accuracy
Answer:
FALSE: Court cases have determined that PBMs are not fiduciaries under ERISA and hence do not face a responsibility to pass savings along to payers (employers, patients and health plans).
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/drugs-regulating-pbms
Answer:
Accountable Community of Health or Accountable Care Communities
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/accountable-communities-health
Answer:
FALSE: A lack of providers in rural areas limits the effectiveness of competition-based, price reduction strategies.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/rural-health
Answer:
Missouri. (Texas, Oklahoma and Wyoming do not have effective rate review).
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/rate-review
Answer:
Maryland
Learn more: https://www.policymed.com/2019/04/scotus-declines-to-get-involved-in-maryland-drug-price-gouging-law.html
Answer:
New Hampshire
Learn more: https://www.hilltopinstitute.org/wp-content/uploads/publications/CommunityBenefitStateLawProfiles-January2015.pdf
Answer:
Delaware
Learn more: https://news.delaware.gov/2018/11/20/executive-order-health-care-spending-quality-benchmarks/
Answer:
Patient Centered Outcomes Research Institute (PCORI)
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/comparative-effectiveness-research
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/telehealth
Answer:
California
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/accountable-care-organizations-acos
Question 25:
According to the Health Care Cost Institute, in what state are patients most likely to get a Surprise Medical Bill?
Answer:
Florida: 26% of in-network admissions resulted in a Surprise Medical Bill in 2016.
Learn more: https://www.healthcostinstitute.org/blog/entry/oon-physician-bills-at-in-network-hospitals
Question 26:
TRUE or FALSE: Antitrust laws effectively preserve healthcare competition.
Answer:
FALSE: Studies have found that antitrust laws are under-enforced, allowing mergers and acquisitions with anti-competitive effects to move forward.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/antitrust-laws
Answer:
14%. Unnecessary/inefficient care is just one form of wasteful healthcare spending, which is estimated to be one third of the nation’s overall healthcare spending.
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/low-value-care
Answer:
TRUE
Learn more: https://nashp.org/trending-now-state-legislation-that-bans-pharmacy-benefit-managers-gag-clauses/
Answer:
Maine and New Hampshire
Learn more: https://www.catalyze.org/wp-content/uploads/2017/11/Price-Transparency-and-Physician-Quality-Report-Card-2017_0-1.pdf
Answer:
TRUE: Moreover, 14% of outpatient visits to the ER and 9% of elective inpatient admissions led to a surprise medical bill.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/surprise-medical-bills
Answer:
90%. Provider concentration was higher than insurer concentration in 58% of markets studied. The opposite was true in only 6% of markets studied.
Learn more: www.commonwealthfund.org/blog/2018/variation-healthcare-provider-and-health-insurer-market-concentration
Question 32:
Name the ONLY state that uses clinical effectiveness to decide what Medicaid should pay for.
Answer:
Oregon: The Health Evidence Review Commission reviews medical evidence in order to prioritize health spending under the Oregon Health Plan and to promote evidence-based medical practice statewide.
Learn more: https://www.oregon.gov/oha/hpa/dsi-herc/Pages/index.aspx
Answer:
Vermont. The state was also the only Round 1 State Innovation Model awardee to realize savings for the Medicare program.
Learn more: https://governor.vermont.gov/press-release/center-medicare-and-medicaid-services-report-recognizes-vermonts-all-payer-health
Answer:
TRUE: “Falls” and procedures performed on the wrong patient/at the wrong site were the 2nd and 3rd most common “never event.”
Learn more: https://www.beckershospitalreview.com/quality/13-statistics-on-never-events.html
Answer:
Prescription drug spending per person increased the most—29% between 2013-2017.
Learn more: https://www.healthcostinstitute.org/research/annual-reports/entry/2017-health-care-cost-and-utilization-report
Answer:
Section 1332 Innovation waiver and Section 1115 Medicaid waiver.
Learn more: https://familiesusa.org/initiatives/waiver-strategy-center
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/advocate-resources/vbid
Answer:
Connecticut
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/office-healthcare-advocate-giving-consumers-seat-table
Question 39:
As of July 2019, how many states have NO protections from surprise medical bills?
Answer:
22 states plus the District of Columbia
Learn more: https://www.commonwealthfund.org/blog/2019/states-are-taking-new-steps-protect-consumers-balance-billing-federal-action-necessary
Question 40:
TRUE or FALSE: A flu shot, prenatal care and eye screening for diabetics are examples of high-value care.
Answer:
TRUE: In some communities we need to increase the provision of high value care.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/high-value-care
Answer:
1985 (It’s time for action!)
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/health-disparities
Answer:
Maryland and Maine
Learn more: https://www.usatoday.com/story/news/health/2019/09/05/drug-prices-how-states-like-colorado-florida-fighting-big-pharma/2213573001/
Answer:
TRUE: In 2013 (the most recent year data was available), the U.S. spent $340 billion on low-value care and $55 billion due to failure to provide high-value care.
Learn more: https://healthcarevaluehub.org/application/files/6315/6358/4957/Hub_Low-Value_vs_High-Value_Care.pdf/
Answer:
Minnesota and California
Learn more: https://www.catalyze.org/wp-content/uploads/2017/11/Price-Transparency-and-Physician-Quality-Report-Card-2017_0-1.pdf/
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/reference-pricing/
Answer:
Either lab or aneshesiology answers are correct. The study looked at this statistic in two ways. (Only one correct answer is needed.)
Learn more: https://www.healthcostinstitute.org/blog/entry/oon-physician-bills-at-in-network-hospitals/
Answer:
Connecticut
Learn more: https://portal.ct.gov/OHS/About/
Answer:
More expensive
Learn more: https://www.jhsph.edu/news/news-releases/2019/us-health-care-spending-highest-among-developed-countries.html
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/application/files/6315/6358/4957/Hub_Low-Value_vs_High-Value_Care.pdf
Answer:
Rhode Island is the only state to incorporate affordability criteria into its annual rate review
Learn more: http://www.ohic.ri.gov/ohic-reformandpolicy-affordability.php
Question 51:
What is the federal agency that grants waivers for state health system transformation activities?
Answer:
The Centers for Medicare & Medicaid Services or CMS. (The Department of Health & Human Services or HHS is okay too).
Learn more: https://innovation.cms.gov/
Answer:
TRUE: Furthermore, the prices of brand name drugs decline to a THIRD of their original cost once FIVE generics enter the market.
Learn more: https://khn.org/news/government-protected-monopolies-drive-drug-prices-higher-study-says/
Question 53:
How many states have COMPREHENSIVE protections from surprise medical bills as of 2019: 6, 13, 25 or 35?
Answer:
13. They are: Washington, Colorado, New Mexico, Texas, California, Connecticut, Florida, Illinois, Maryland, New Hampshire, New Jersey, New York and Oregon.
Learn more: https://www.commonwealthfund.org/blog/2019/states-are-taking-new-steps-protect-consumers-balance-billing-federal-action-necessary
Question 54:
TRUE or FALSE: Price transparency drives smarter spending by consumers.
Answer:
FALSE: Other audiences (like policmakers, regulators and providers) are better-positioned to drive value by making use of this information.
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/revealing-truth-about-healthcare-price-transparency
Answer:
TRUE: New codes will help doctors, social workers, care managers and others document patients’ social history along with their medical history.
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/social-determinants-health
Answer:
Colorado
Learn more: https://www.thedenverchannel.com/news/politics/colorado-gov-polis-creates-office-of-saving-people-money-on-health-care-through-executive-order
Question 57:
According to just about every survey, what is consumers’ top healthcare-related concern?
Answer:
Possible answers: costs, affordability or prices
Learn more: https://www.kff.org/health-costs/issue-brief/data-note-americans-challenges-health-care-costs/
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/surprise-medical-bills
Answer:
Possible answers: Bundled payments, capitation, global budgets, pay-for-performance, shared savings, value-based purchasing.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/provider-payment-reform
Answer:
Oregon, with 58% of hospitals receiving an “A” rating.
Learn more: https://www.hospitalsafetygrade.org/your-hospitals-safety-grade/state-rankings
Question 61:
TRUE or FALSE: Hospital mergers increase the price of a hospital stay.
Answer:
TRUE: A 2018 analysis found that prices in most areas increase between 11 and 54 percent in the years following the merger.
Learn more: https://www.nytimes.com/2018/11/14/health/hospital-mergers-health-care-spending.html
Answer:
Oklahoma
Learn more: https://www.businessinsider.com/oklahomas-new-medicaid-only-pay-for-working-drugs-2018-8
Question 63:
Name two PERSONAL determinants of health (as opposed to SOCIAL determinants of health).
Answer:
Possible answers: Genetics, smoking, sedentary lifestyle, poor eating habits or any other personal behavior that negatively affects health.
Learn more: https://healthcarevaluehub.org/cost-drivers
Answer:
FALSE: These states had the LOWEST percentages of hospitals receiving an “A” rating within the U.S.
Learn more: https://www.hospitalsafetygrade.org/your-hospitals-safety-grade/state-rankings
Answer:
Washington
Learn more: https://www.seattletimes.com/seattle-news/health/under-new-washington-law-state-will-invest-more-in-improving-native-american-tribal-members-health/
Answer:
TRUE: The actual cost of low-value services is likely much higher - the study analyzed only 47 (out of 550) tests/procedures that should be questioned.
Learn more: https://www.wacommunitycheckup.org/media/47156/2018-first-do-no-harm.pdf
Answer:
D) All of the above
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/provider-shortages
Answer:
Possible answers: Colorado, Delaware, Maryland, Massachusetts, Oregon, Pennsylvania, Vermont, Virginia
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/health-system-oversight-states-environmental-scan
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/health-disparities
Question 70:
Approximately what portion of spending for healthcare services is considered “shoppable:” 13, 33, 53 or 63 percent?
Answer:
Depending on the source, 33-43%. If we look at spending that is shoppable AND paid out-of-pocket, the amount is closer to 7%.
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/revealing-truth-about-healthcare-price-transparency
Answer:
Possible answers: AK, AR, AZ, CA, CO, CT, DC, DE, HI, IA, IL, IN, KY, LA, MA, MD, ME, MI, MN, MT, ND, NH, NJ, NM, NV, NY, OH, OR, PA, RI, VA, VE, WA, WV.
Learn more: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
Question 72:
Name the TWO major components of healthcare “value:” A) quality, B) cost, C) accountability
Answer:
A and B: quality and cost
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems
Answer:
$78
Learn more: https://healthcarevaluehub.org/application/files/2115/6304/2921/Hub_Eggs_vs_Medical_Final.pdf
Question 74:
TRUE or FALSE: National healthcare expenditures could be greatly reduced by eliminating health disparities.
Answer:
TRUE: A 2018 report by Altarum and the W.K. Kellogg Foundation estimated that the U.S. spends $93 billion in excess medical costs per year as a result of health disparities.
Learn more: https://altarum.org/RacialEquity2018
Answer:
Lack of diet soda in hospital cafeteria is not a form of medical harm.
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/medical-harm
Question 76:
Name three SOCIAL determinants of health.
Answer:
Possible answers: Lack of transportation, lack of access to healthy foods, poor housing conditions, lack of education, unemployment, adverse childhood experiences/trauma.
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/browse-cost-driverquality-issue/social-determinants-health
Answer:
FALSE: Research shows that high-deductible health plans cause consumers to cut back on both necessary and unnecessary care, as well as leaving them with unmanageable amounts of medical debt.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/high-deductible-health-planshealth-savings-accounts-hsas
Answer:
C: 34%
Learn more: https://www.kff.org/health-costs/issue-brief/data-note-americans-challenges-health-care-costs/
Question 79:
TRUE or FALSE: Fee-for-service is appropriate for some types of healthcare services.
Answer:
TRUE: High-value services that we want to see more of, like a flu shot, are well-suited for fee-for-serivce payments.
Learn more: https://healthcarevaluehub.org/application/files/8015/6365/1789/NOLA_Report_Final_Website
Answer:
C) 69%
Learn more: https://www.gao.gov/assets/700/697684.pdf
Answer:
Louisiana, Maine and Minnesota. The move was aimed at Pharmacy Benefit Managers who “claw back” the extra dollars from pharmacists.
Learn more: https://www.leavenworthtimes.com/news/20190913/kansas-lawmakers-looking-to-other-states-for-ways-to-control-health-costs
Answer:
FALSE: A review of large employer wellness programs found that health screenings and lifestyle management programs aimed at smoking cessation or disease prevention did not significantly reduce healthcare costs or utilization. Disease management programs targeted exclusively at people with chronic illness may generate more meaningful savings.
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/wellness-programs-and-incentives-review-evidence
Answer:
D) All of the above
Learn more: https://healthcarevaluehub.org/cost-and-quality-problems/why-urgent-problem
Answer:
TRUE
Learn more: https://www.communitycatalyst.org/resources/publications/document/Community-Catalyst-CHW-Issue-Brief.pdf
Answer:
Missouri
Learn more: https://khn.org/news/why-missouris-the-last-holdout-on-a-statewide-rx-monitoring-program/
Answer:
TRUE: This finding from the Urban Institute suggests that currently high levels of insurance among children do not protect them from family financial insecurity due to medical bills.
Learn more: https://www.urban.org/research/publication/despite-recent-improvement-one-six-children-lived-family-problems-paying-medical-bills-2017
Answer:
New York. The most concentrated markets were in metro areas with populations of less than 300,000 (as of 2016).
Learn more: https://www.healthcostinstitute.org/research/hmi/hmi-interactive#HMI-Concentration-Index
Answer:
TRUE
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/making-healthcare-affordable-finding-common-approach-measure-progress
Answer:
Virginia will pay out the highest total rebates, followed by Pennsylvania and Florida.
Learn more: https://www.kff.org/private-insurance/issue-brief/data-note-2019-medical-loss-ratio-rebates/
Answer:
TRUE: Black and Hispanic Medicare patients were more likely to be transported to a safety-net emergency department.
Learn more: https://www.fiercehealthcare.com/hospitals-health-systems/white-medicare-patients-transported-to-closest-ed-more-often-than-blacks
Answer:
Mixed, partially reflecting a diversity of approaches.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/accountable-care-organizations-acos
Answer:
TRUE (‘nuff said)
Learn more: https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-august-2019/
Answer:
TRUE: Our understanding of best practices for designing and using screening tools increases every day.
Learn more: https://healthleadsusa.org/resources/the-health-leads-screening-toolkit/
Question 94:
The U.S. spends more per person on healthcare than other developed countries. Do we get higher quality as a result?
Answer:
No!
Learn more: https://www.healthsystemtracker.org/chart-collection/quality-u-s-healthcare-system-compare-countries/
Answer:
TRUE, although wide variation in approaches suggests we should be cautious about making generalizations.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/accountable-communities-health
Answer:
Weak. There are better interventions for inducing provider practice changes.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/malpractice-reform
Question 97:
TRUE or FALSE: Patient shared decision making is widely practiced and considered a standard of care.
Answer:
FALSE: Despite strong evidence of patient benefits, shared decision-making has not been widely implemented in clinical practice.
Learn more: https://healthcarevaluehub.org/advocate-resources/publications/consumer-benefits-patient-shared-decision-making/
Answer:
TRUE: Many states have passed legislation to expand non-physician providers’ “scope of practice” to alleviate physician shortages.
Learn more: https://healthcarevaluehub.org/improving-value/browse-strategy/provider-scope-practice